Chapter 4: Immunity
Learning Objectives
By the end of this section, you will be able to:
- Describe physical and chemical immune barriers
- Explain innate immune responses
- Explain adaptive immunity
- Compare and contrast adaptive and innate immunity
- Explain how vaccines work
Organisms have a wide array of adaptations for preventing attacks of parasites and diseases. The human defense system is complex, multilayered, and has unique defenses. These unique defenses interact with other defense systems inherited from ancestral lineages, and include complex and specific pathogen recognition and memory mechanisms. Research continues to unravel the complexities and vulnerabilities of the immune system.
Immunity
The environment consists of numerous pathogens, which are agents, usually microorganisms, that cause diseases in their hosts. A host is the organism that is invaded and often harmed by a pathogen. Pathogens include bacteria, fungi and other infectious organisms. We are constantly exposed to pathogens in food and water, on surfaces, and in the air. The immune systems for mammals evolved for protection from such pathogens; they are composed of an extremely diverse array of specialized cells and soluble molecules that coordinate a rapid and flexible defense system capable of providing protection from a majority of these disease agents.
Components of the immune system constantly search the body for signs of pathogens. When pathogens are found, immune factors are mobilized to the site of an infection. The immune factors identify the nature of the pathogen, strengthen the corresponding cells and molecules to combat it efficiently, and then halt the immune response after the infection is cleared to avoid unnecessary cell damage in the host. The immune system can remember pathogens to which it has been exposed to create a more efficient response upon re-exposure. This memory can last several decades. Features of the immune system, such as pathogen identification, specific response, amplification, retreat, and remembrance are essential for survival against pathogens. The immune response can be classified as either innate or adaptive. The innate immune response is always present and attempts to defend against all pathogens rather than focusing on specific ones. Conversely, the adaptive immune response stores information about past infections and mounts pathogen-specific defenses. There is also a third type of immunity called passive immunity. This occurs when immunity is b’borrowed’ from another source, and often only lasts a short time.
Innate Immunity
Innate immunity occurs naturally because of genetic factors or physiology; it is not induced by infection or vaccination but works to reduce the workload for the adaptive immune response. It is a general response to pathogens. The innate immune system developed early in animal evolution, roughly a billion years ago, as an essential response to infection. Innate immunity has a limited number of specific targets: any pathogenic threat triggers a consistent sequence of events that can identify the type of pathogen and either clear the infection independently or mobilize a highly specialized adaptive immune response. For example, tears and mucus secretions contain microbicidal factors (agents that kills microscopic organisms). Other examples of innate immunity include the skin, which acts as a physical barrier, the cough reflex, and stomach acids.
Adaptive Immunity
The adaptive, or acquired, immune response takes days or even weeks to become established—much longer than the innate response; however, adaptive immunity is more specific to pathogens and has memory. Adaptive immunity is an immunity that occurs after exposure to an antigen either from a pathogen or a vaccination. This part of the immune system is activated when the innate immune response is insufficient to control an infection. In fact, without information from the innate immune system, the adaptive response could not be mobilized. The response is specific to the pathogen, and produces antibodies specific to that pathogen. Adaptive immunity also involves a memory to provide the host with long-term protection from reinfection with the same type of pathogen; on re-exposure, this memory will facilitate an efficient and quick response.
Passive Immunity
The passive immune response last only a short time. This immunity is ‘borrowed’ from another source. For example, a newborn baby benefits from the mother’s antibodies found in her breast milk. These antibodies can protect the infant from diseases the mother has encountered and for which she has produced antibodies.
Vaccines
Despite a poor understanding of the workings of the body in the early 18th century in Europe, the practice of inoculation as a method to prevent the often-deadly effects of smallpox was introduced from the courts of the Ottoman Empire. The method involved causing limited infection with the smallpox virus by introducing the pus of an affected individual to a scratch in an uninfected person. The resulting infection was milder than if it had been caught naturally and mortality rates were shown to be about two percent rather than 30 percent from natural infections. Moreover, the inoculation gave the individual immunity to the disease. It was from these early experiences with inoculation that the methods of vaccination were developed, in which a weakened or relatively harmless (killed) derivative of a pathogen is introduced into the individual. The vaccination induces immunity to the disease with few of the risks of being infected. A modern understanding of the causes of the infectious disease and the mechanisms of the immune system began in the late 19th century and continues to grow today.
Vaccinologist
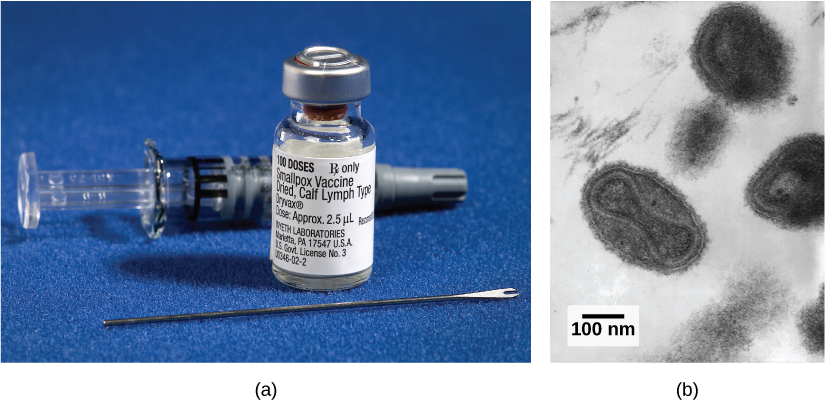
Vaccination (or immunization) involves the delivery, usually by injection as shown in Figure 4.2, of noninfectious antigen(s) derived from known pathogens. Other components are delivered at the same time to help stimulate the immune response. Immunological memory is the reason vaccines work. Ideally, the effect of vaccination is to elicit immunological memory, and thus resistance to specific pathogens without the individual having to experience an infection. By introducing a weakened or harmless form of the pathogen, the immune response is to produce antibodies against that antigen. These antibodies stay in the body and serve as memory to fight off this specific pathogen in the future.

Vaccinologists are involved in the process of vaccine development from the initial idea to the availability of the completed vaccine. This process can take decades, can cost millions of dollars, and can involve many obstacles along the way. For instance, injected vaccines stimulate the systemic immune system, eliciting humoral and cell-mediated immunity, but have little effect on the mucosal response, which presents a challenge because many pathogens are deposited and replicate in mucosal compartments, and the injection does not provide the most efficient immune memory for these disease agents. For this reason, vaccinologists are actively involved in developing new vaccines that are applied via intranasal, aerosol, oral, or transcutaneous (absorbed through the skin) delivery methods. Importantly, mucosal-administered vaccines elicit both mucosal and systemic immunity and produce the same level of disease resistance as injected vaccines.

Summary
The innate immune system serves as a first responder to pathogenic threats that bypass natural physical and chemical barriers of the body. Using a combination of cellular and molecular attacks, the innate immune system identifies the nature of a pathogen and responds. When innate mechanisms are insufficient to clear an infection, the adaptive immune response is informed and mobilized. The adaptive immune response is a slower-acting, longer-lasting, and more specific response than the innate response. However, the adaptive response requires information from the innate immune system to function. Vaccines use the adaptive immune response to create antibodies against specific pathogens to protect the organism from future attacks.
Glossary
adaptive immunity: immunity that has memory and occurs after exposure to an antigen either from a pathogen or a vaccination antigen: foreign or “non-self” protein that triggers the immune response
antibody: a protective protein produced by the immune system in response to the presence of a foreign substance
host: an organism that is invaded by a pathogen or parasite
innate immunity: immunity that occurs naturally because of genetic factors or physiology, and is not induced by infection or vaccination
passive immunity: immunity borrowed from another source
pathogen: an agent, usually a microorganism, that causes disease in the organisms that they invade
vaccination: the process by which a weakened or harmless derivative of a pathogen is introduced in order to produce an immune response and so the organism may produce antibodies as protection

