Chapter 9: Human Reproduction
Learning Objectives
By the end of this section, you will be able to:
- Describe human male and female reproductive anatomies
- Describe the roles of male and female reproductive hormones
- Describe the processes of gestation and labour
As in all animals, the adaptations for reproduction in humans are complex. They involve specialized and different anatomies in the two sexes, a hormone regulation system, and specialized behaviors regulated by the brain and endocrine system.
The Human Reproductive System
The reproductive tissues of male and female humans develop similarly in utero until about the seventh week of gestation when a low level of the hormone testosterone is released from the gonads of the developing male. Testosterone causes the primitive gonads to differentiate into male sexual organs. When testosterone is absent, the primitive gonads develop into ovaries. Tissues that produce a penis in males produce a clitoris in females. The tissue that will become the scrotum in a male becomes the labia in a female. Thus the male and female anatomies arise from a divergence in the development of what were once common embryonic structures.
Male Reproductive Anatomy
Sperm are immobile at body temperature; therefore, the testes are external to the body so that a correct temperature is maintained for motility. In humans, the pair of testes must be suspended outside the body so the environment of the sperm is about 2 °C lower than body temperature to produce viable sperm. If the testes do not descend through the abdominal cavity during fetal development, the individual has reduced fertility.
The scrotum houses the testicles or testes (singular: testis), and provides passage for blood vessels, nerves, and muscles related to testicular function. The testes are a pair of male gonads that produce sperm and reproductive hormones. Each testis is approximately 2.5 by 3.8 cm (1.5 by 1 inch) in size and divided into wedge-shaped lobes by septa. Coiled in each wedge are seminiferous tubules that produce sperm.
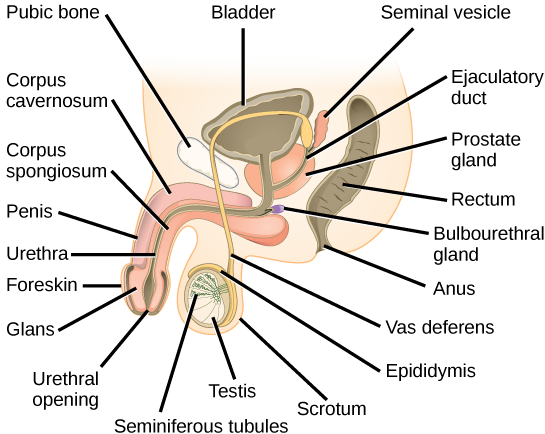
The penis drains urine from the urinary bladder and is a copulatory organ during intercourse (Figure 9.1, Table 9.1). The penis contains three tubes of erectile tissue that become engorged with blood, making the penis erect, in preparation for intercourse. The organ is inserted into the vagina culminating with an ejaculation. During orgasm, the accessory organs and glands connected to the testes contract and empty the semen (containing sperm) into the urethra and the fluid is expelled from the body by muscular contractions causing ejaculation. After intercourse, the blood drains from the erectile tissue and the penis becomes flaccid.
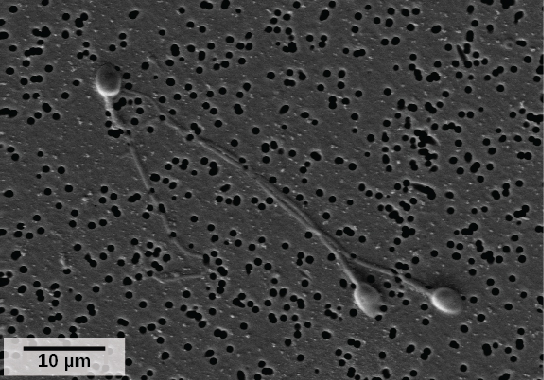
Semen is a mixture of sperm (about five percent of the total) and fluids from accessory glands that contribute most of the semen’s volume. Sperm are the male reproductive cells, consisting of a flagellum for motility, a neck that contains the cell’s energy-producing mitochondria, and a head that contains the genetic material (Figure 9.2). At the top of the head of the sperm is the acrosome, a structure containing enzymes that can digest the protective coverings that surround the egg and allow the sperm to fuse with the egg. An ejaculate will contain from two to five milliliters of fluid and from 50–120 million sperm per milliliter.
Sperm form in the walls of seminiferous tubules that are coiled inside the testes (Figure 9.1, Table 9.1). When the sperm have developed flagella they leave the seminiferous tubules and enter the epididymis (Figure 9.1, Table 9.1). This structure lies along the top and posterior of the testes and is the site of sperm maturation. The sperm leave the epididymis and enter the vas deferens, which carries the sperm behind the bladder, and forms the ejaculatory duct with the duct from the seminal vesicles. During a vasectomy, a section of the vas deferens is removed, preventing sperm (but not the secretions of the accessory glands) from being passed out of the body during ejaculation and preventing fertilization.
The bulk of the semen comes from the accessory glands associated with the male reproductive system. These are the seminal vesicles, the prostate gland, and the bulbourethral gland (Figure 9.1, Table 9.1). The secretions from the accessory glands provide important compounds for the sperm including nutrients, electrolytes, and pH buffering. There are also coagulation factors that affect sperm delivery and motility.
| Organ | Location | Function |
|---|---|---|
| Scrotum | External | Supports testes and regulates their temperature |
| Penis | External | Delivers urine, copulating organ |
| Testes | Internal | Produce sperm and male hormones |
| Seminal Vesicles | Internal | Contribute to semen production |
| Prostate Gland | Internal | Contributes to semen production |
| Bulbourethtral Glands | Internal | Neutralize urine in urethra |
Female Reproductive Anatomy
Internal female reproductive structures include ovaries, oviducts, the uterus, and the vagina (Figure 9.3, Table 9.2). The pair of ovaries is held in place in the abdominal cavity by a system of ligaments. The outermost layer of the ovary is made up of follicles, each consisting of one or more follicular cells that surround, nourish, and protect a single egg. During the menstrual period, a batch of follicular cells develops and prepares their eggs for release. At ovulation, one follicle ruptures and one egg is released. Following ovulation, the follicular tissue that surrounded the ovulated egg stays within the ovary and grows to form a solid mass called the corpus luteum. The corpus luteum secretes additional estrogen and the hormone progesterone that helps maintain the uterine lining during pregnancy. The ovaries also produce hormones, such as estrogen.
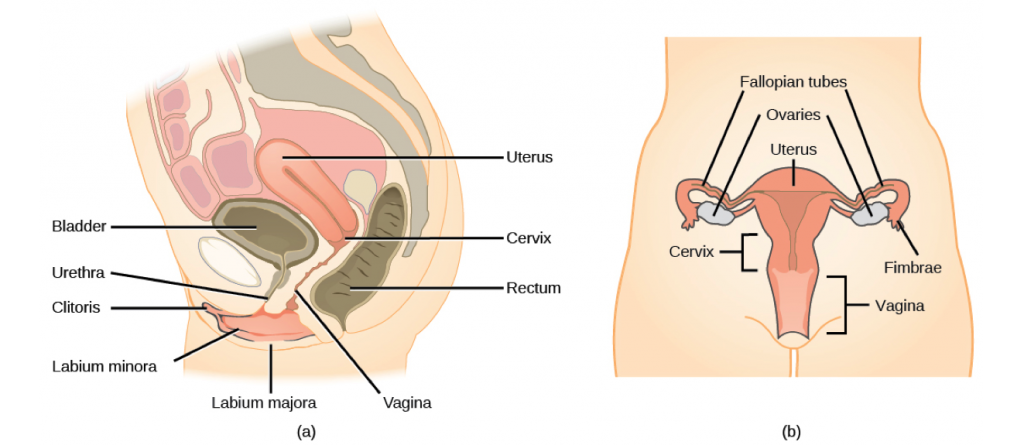
The oviducts, or fallopian tubes, extend from the uterus in the lower abdominal cavity to the ovaries, but they are not in contact with the ovaries. The lateral ends of the oviducts flare out into a trumpet-like structure and have a fringe of finger-like projections called fimbrae (Figure 9.3b). When an egg is released at ovulation, the fimbrae help the nonmotile egg enter into the tube. The walls of the oviducts have a ciliated epithelium over smooth muscle. The cilia beat, and the smooth muscle contracts, moving the egg toward the uterus. Fertilization usually takes place within the oviduct and the developing embryo is moved toward the uterus. It usually takes the egg or embryo a week to travel through the oviduct.
Sterilization in women is called a tubal ligation; it is analogous to a vasectomy in males in that the oviducts are severed and sealed, preventing sperm from reaching the egg.
The uterus is a structure about the size of a woman’s fist. The uterus has a thick muscular wall and is lined with an endometrium rich in blood vessels and mucus glands that develop and thicken during the female cycle. Thickening of the endometrium prepares the uterus to receive the fertilized egg or zygote, which will then implant itself in the endometrium. The uterus supports the developing embryo and fetus during gestation. Contractions of the smooth muscle in the uterus aid in forcing the baby through the vagina during labor. If fertilization does not occur, a portion of the lining of the uterus sloughs off during each menstrual period. The endometrium builds up again in preparation for implantation. Part of the uterus, called the cervix, protrudes into the top of the vagina.
The vagina is a muscular tube that serves several purposes. It allows menstrual flow to leave the body. It is the receptacle for the penis during intercourse and the pathway for the delivery of offspring.
The breasts consist of mammary glands and fat. Each gland consists of 15 to 25 lobes that have ducts that empty at the nipple and that supply the nursing child with nutrient- and antibody-rich milk to aid development and protect the child.
| Organ | Location | Function |
|---|---|---|
| Clitoris | External | Sensory organ |
| Mons pubis | External | Fatty area overlying pubic bone |
| Labia majora | External | Covers labia minora; contains sweat and sebaceous glands |
| Labia minora | External | Covers vestibule |
| Greater vestibular glands | External | Secrete mucus; lubricate vagina |
| Breast | External | Produces and delivers milk |
| Ovaries | Internal | Produce and develop eggs |
| Oviducts | Internal | Transport egg to uterus; site of fertilization |
| Uterus | Internal | Supports developing embryo |
| Vagina | Internal | Common tube for intercourse, birth canal, passing menstrual flow |
Hormonal Control of Reproduction
The human male and female reproductive cycles are controlled by the interaction of hormones from the hypothalamus and anterior pituitary with hormones from reproductive tissues and organs. In both sexes, the hypothalamus monitors and causes the release of hormones from the anterior pituitary gland. When the reproductive hormone is required, the hypothalamus sends a gonadotropin-releasing hormone (GnRH) to the anterior pituitary. This causes the release of follicle stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary into the blood. Although these hormones are named after their functions in female reproduction, they are produced in both sexes and play important roles in controlling reproduction. Other hormones have specific functions in the male and female reproductive systems.
Male Hormones
At the onset of puberty, the hypothalamus causes the release of FSH and LH into the male system for the first time. FSH enters the testes and stimulates the Sertoli cells located in the walls of the seminiferous tubules to begin promoting spermatogenesis. LH also enters the testes and stimulates the interstitial cells of Leydig, located in between the walls of the seminiferous tubules, to make and release testosterone into the testes and the blood.
Testosterone stimulates spermatogenesis. This hormone is also responsible for the secondary sexual characteristics that develop in the male during adolescence. The secondary sex characteristics in males include a deepening of the voice, the growth of facial, axillary, and pubic hair, an increase in muscle bulk, and the beginnings of the sex drive.
Female Hormones
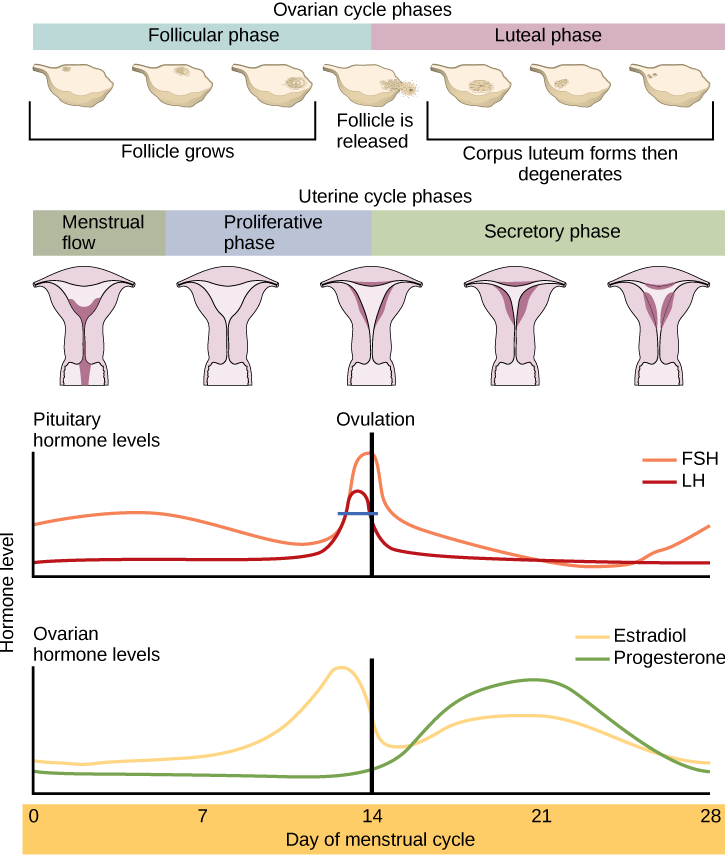
The control of reproduction in females is more complex. The female reproductive cycle is divided into the ovarian cycle and the menstrual cycle. The ovarian cycle governs the preparation of endocrine tissues and release of eggs, while the menstrual cycle governs the preparation and maintenance of the uterine lining. These cycles are coordinated over a 22–32 day cycle, with an average length of 28 days.
As with the male, the GnRH from the hypothalamus causes the release of the hormones FSH and LH from the anterior pituitary. In addition, estrogen and progesterone are released from the developing follicles. As with testosterone in males, estrogen is responsible for the secondary sexual characteristics of females. These include breast development, flaring of the hips, and a shorter period for bone growth.
The ovarian and menstrual cycles are regulated by hormones of the hypothalamus, pituitary, and ovaries. The ebb and flow of the hormones causes the ovarian and menstrual cycles to advance. The ovarian and menstrual cycles occur concurrently. The first half of the ovarian cycle is the follicular phase. Slowly rising levels of FSH cause the growth of follicles on the surface of the ovary. This process prepares the egg for ovulation. As the follicles grow, they begin releasing estrogen. The first few days of this cycle coincide with menstruation or the sloughing off of the functional layer of the endometrium in the uterus. After about five days, estrogen levels rise and the menstrual cycle enters the proliferative phase. The endometrium begins to regrow, replacing the blood vessels and glands that deteriorated during the end of the last cycle.
Just prior to the middle of the cycle (approximately day 14), the high level of estrogen causes FSH and especially LH to rise rapidly then fall. The spike in LH causes the most mature follicle to rupture and release its egg. This is ovulation. The follicles that did not rupture degenerate and their eggs are lost. The level of estrogen decreases when the extra follicles degenerate.
Following ovulation, the ovarian cycle enters its luteal phase, and the menstrual cycle enters its secretory phase, both of which run from about day 15 to 28. The luteal and secretory phases refer to changes in the ruptured follicle. The cells in the follicle undergo physical changes and produce a structure called a corpus luteum. The corpus luteum produces estrogen and progesterone. The progesterone facilitates the regrowth of the uterine lining and inhibits the release of further FSH and LH. The uterus is being prepared to accept a fertilized egg, should it occur during this cycle. The inhibition of FSH and LH prevents any further eggs and follicles from developing, while the progesterone is elevated. The level of estrogen produced by the corpus luteum increases to a steady level for the next few days.
If no fertilized egg is implanted into the uterus, the corpus luteum degenerates and the levels of estrogen and progesterone decrease. The endometrium begins to degenerate as the progesterone levels drop, initiating the next menstrual cycle. The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles again. Figure 9.4 visually compares the ovarian and uterine cycles as well as the commensurate hormone levels.
Gestation
Pregnancy begins with the fertilization of an egg and continues through to the birth of the individual. The length of time of gestation, or the gestation period, in humans is 266 days and is similar in other great apes.
Within 24 hours of fertilization, the egg and sperm nuclei fuse and the cell is known as a zygote. The zygote initiates cleavage, developing into a greater number of cells, and the developing embryo travels through the oviduct to the uterus (Figure 9.5). The developing embryo must implant into the wall of the uterus within seven days, or it will deteriorate and die. The outer layers of the developing embryo or blastocyst grow into the endometrium by digesting the endometrial cells, and healing of the endometrium closes up the blastocyst into the tissue. Another layer of the blastocyst, the chorion, begins releasing a hormone called human beta chorionic gonadotropin (β-HCG), which makes its way to the corpus luteum and keeps that structure active. This ensures adequate levels of progesterone that will maintain the endometrium of the uterus for the support of the developing embryo. Pregnancy tests determine the level of β-HCG in urine or serum. If the hormone is present, the test is positive.
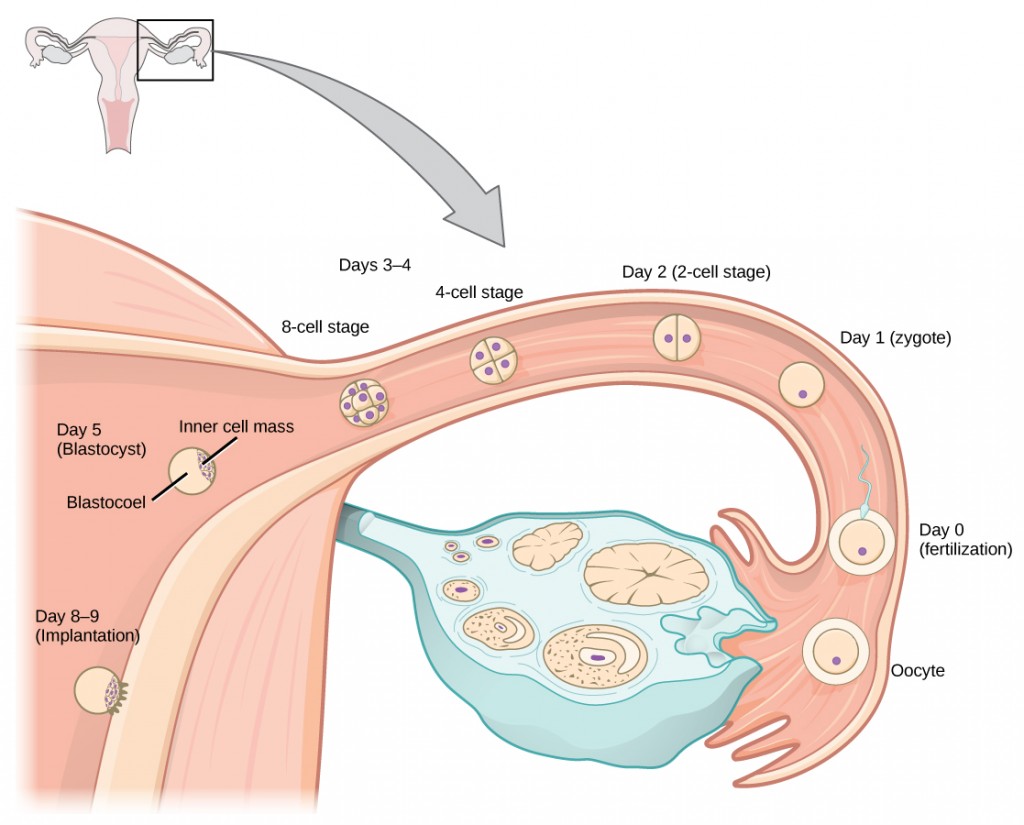
The gestation period is divided into three equal periods or trimesters. During the first two-to-four weeks of the first trimester, nutrition and waste are handled by the endometrial lining through diffusion. As the trimester progresses, the outer layer of the embryo begins to merge with the endometrium, and the placenta forms. The placenta takes over the nutrient and waste requirements of the embryo and fetus, with the mother’s blood passing nutrients to the placenta and removing waste from it. Chemicals from the fetus, such as bilirubin, are processed by the mother’s liver for elimination. Some of the mother’s immunoglobulins will pass through the placenta, providing passive immunity against some potential infections.
Internal organs and body structures begin to develop during the first trimester. By five weeks, limb buds, eyes, the heart, and liver have been basically formed. By eight weeks, the term fetus applies, and the body is essentially formed (Figure 9.6a). The individual is about five centimeters (two inches) in length and many of the organs, such as the lungs and liver, are not yet functioning. Exposure to any toxins is especially dangerous during the first trimester, as all of the body’s organs and structures are going through initial development. Anything that interferes with chemical signaling during that development can have a severe effect on the fetus’ survival.
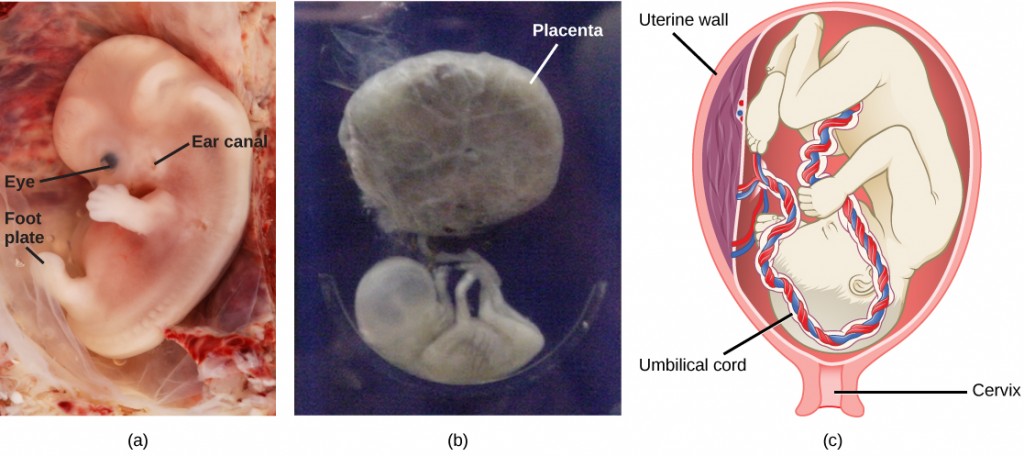
During the second trimester, the fetus grows to about 30 cm (about 12 inches) (Figure 9.6b). It becomes active and the mother usually feels the first movements. All organs and structures continue to develop. The placenta has taken over the functions of nutrition and waste elimination and the production of estrogen and progesterone from the corpus luteum, which has degenerated. The placenta will continue functioning up through the delivery of the baby. During the third trimester, the fetus grows to 3 to 4 kg (6.5–8.5 lbs.) and about 50 cm (19–20 inches) long (Figure 9.6c). This is the period of the most rapid growth during the pregnancy as all organ systems continue to grow and develop.
Labor is the muscular contractions to expel the fetus and placenta from the uterus. Toward the end of the third trimester, estrogen causes receptors on the uterine wall to develop and bind the hormone oxytocin. At this time, the baby reorients, facing forward and down with the back or crown of the head engaging the cervix (uterine opening). This causes the cervix to stretch and nerve impulses are sent to the hypothalamus, which signals the release of oxytocin from the posterior pituitary. Oxytocin causes smooth muscle in the uterine wall to contract. At the same time, the placenta releases prostaglandins into the uterus, increasing the contractions. As more smooth muscle cells are recruited, the contractions increase in intensity and force.
There are three stages to labor. During stage one, the cervix thins and dilates. This is necessary for the baby and placenta to be expelled during birth. The cervix will eventually dilate to about 10 cm. During stage two, the baby is expelled from the uterus. The uterus contracts and the mother pushes as she compresses her abdominal muscles to aid the delivery. The last stage is the passage of the placenta after the baby has been born and the organ has completely disengaged from the uterine wall. If labor should stop before stage two is reached, synthetic oxytocin, known as Pitocin, can be administered to restart and maintain labor.
Infertility
Infertility is the inability to conceive a child or carry a child to birth. About 75 percent of causes of infertility can be identified. These include diseases, such as sexually transmitted diseases that can cause scarring of the reproductive tubes in either men or women, or developmental problems frequently related to abnormal hormone levels in one of the individuals. Inadequate nutrition, especially starvation, can delay menstruation. Stress can also lead to infertility. Short-term stress can affect hormone levels, while long-term stress can delay puberty and cause less frequent menstrual cycles. Other factors that affect fertility include toxins (such as cadmium), tobacco smoking, marijuana use, gonadal injuries, and aging.
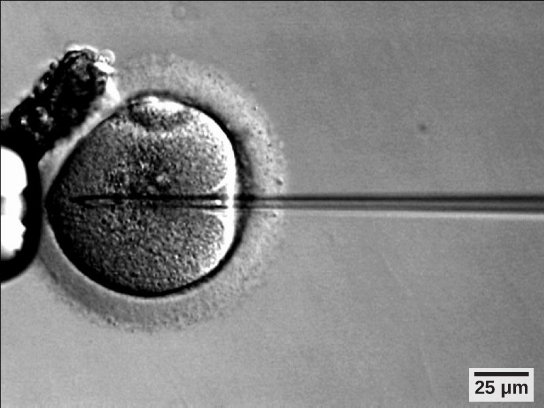
If infertility is identified, several assisted reproductive technologies (ART) are available to aid conception. A common type of ART is in vitro fertilization (IVF) where an egg and sperm are combined outside the body and then placed in the uterus. Eggs are obtained from the woman after extensive hormonal treatments that prepare mature eggs for fertilization and prepare the uterus for implantation of the fertilized egg. Sperm are obtained from the man and they are combined with the eggs and supported through several cell divisions to ensure viability of the zygotes. When the embryos have reached the eight-cell stage, one or more is implanted into the woman’s uterus. If fertilization is not accomplished by simple IVF, a procedure that injects the sperm into an egg can be used. This is called intracytoplasmic sperm injection (ICSI) (Figure 9.7). IVF procedures produce a surplus of fertilized eggs and embryos that can be frozen and stored for future use. The procedures can also result in multiple births.
Reproductive Endocrinologist
A reproductive endocrinologist is a physician who treats a variety of hormonal disorders related to reproduction and infertility in both men and women. The disorders include menstrual problems, infertility, pregnancy loss, sexual dysfunction, and menopause. Doctors may use fertility drugs, surgery, or assisted reproductive techniques (ART) in their therapy. Reproductive endocrinologists undergo extensive medical training, first in a four-year residency in obstetrics and gynecology, then in a three-year fellowship in reproductive endocrinology. To be board certified in this area, the physician must pass written and oral exams in both areas.
Summary
The reproductive structures that evolved in humans allow males and females to mate, fertilize internally, and support the growth and development of offspring.
The male and female reproductive cycles are controlled by hormones released from the hypothalamus and anterior pituitary and hormones from reproductive tissues and organs. The hypothalamus monitors the need for FSH and LH production and release from the anterior pituitary. FSH and LH affect reproductive structures to cause the formation of sperm in males and the preparation of eggs for release in females and possible fertilization.
Human pregnancy begins with fertilization of an egg and proceeds through the three trimesters of gestation. The first trimester lays down the basic structures of the body, including the limb buds, heart, eyes, and the liver. The second trimester continues the development of all of the organs and systems. The third trimester exhibits the greatest growth of the fetus and culminates in labor and delivery. The labor process has three stages (contractions, delivery of the fetus, and expulsion of the placenta), each propelled by hormones.
Exercises
- Which of the following statements about the male reproductive system is false?
- The vas deferens carries sperm from the testes to the seminal vesicles.
- The ejaculatory duct joins the urethra.
- Both the prostate and the bulbourethral glands produce components of the semen.
- The prostate gland is located in the testes.
- Which of the following statements about hormone regulation of the female reproductive cycle is false?
- LH and FSH are produced in the pituitary, and estrogen and progesterone are produced in the ovaries.
- Estradiol and progesterone secreted from the corpus luteum cause the endometrium to thicken.
- Both progesterone and estrogen are produced by the follicles.
- Secretion of GnRH by the hypothalamus is inhibited by low levels of estrogen but stimulated by high levels of estrogen.
- Sperm are produced in the ________.
- scrotum
- seminal vesicles
- seminiferous tubules
- prostate gland
- Which female organ has an endometrial lining that will support a developing baby?
- labia minora
- breast
- ovaries
- uterus
- Which hormone causes FSH and LH to be released?
- testosterone
- estrogen
- GnRH
- progesterone
- Nutrient and waste requirements for the developing fetus are handled during the first few weeks by ________.
- the placenta
- diffusion through the endometrium
- the chorion
- the blastocyst
- Which hormone is primarily responsible for the contractions during labor?
- oxytocin
- estrogen
- β-HCG
- progesterone
- Describe the events in the ovarian cycle leading up to ovulation.
- Describe the stages of labor.
Answers
- D
- C
- C
- D
- C
- B
- A
- Low levels of progesterone allow the hypothalamus to send GnRH to the anterior pituitary and cause the release of FSH and LH. FSH stimulates follicles on the ovary to grow and prepare the eggs for ovulation. As the follicles increase in size, they begin to release estrogen and a low level of progesterone into the blood. The level of estrogen rises to a peak, causing a spike in the concentration of LH. This causes the most mature follicle to rupture and ovulation occurs.
- Stage one of labor results in uterine contractions, which thin the cervix and dilate the cervical opening. Stage two delivers the baby, and stage three delivers the placenta.
Glossary
bulbourethral gland: the paired glands in the human male that produce a secretion that cleanses the urethra prior to ejaculation
corpus luteum: the endocrine tissue that develops from an ovarian follicle after ovulation; secretes progesterone and estrogen during pregnancy
estrogen: a reproductive hormone in females that assists in endometrial regrowth, ovulation, and calcium absorption
follicle stimulating hormone (FSH): a reproductive hormone that causes sperm production in men and follicle development in women
gestation: the development before birth of a viviparous animal
gestation period: the length of time of development, from conception to birth, of the young of a viviparous animal
gonadotropin-releasing hormone (GnRH): a hormone from the hypothalamus that causes the release of FSH and LH from the anterior pituitary
human beta chorionic gonadotropin (β-HCG): a hormone produced by the chorion of the zygote that helps to maintain the corpus luteum and elevated levels of progesterone
infertility: the inability to conceive, carry or deliver children
luteinizing hormone (LH): a reproductive hormone in both men and women, causes testosterone production in men and ovulation and lactation in women
menstrual cycle: the cycle of the degradation and re-growth of the endometrium
ovarian cycle: the cycle of preparation of egg for ovulation and the conversion of the follicle to the corpus luteum
oviduct: (also, fallopian tube) the muscular tube connecting uterus with ovary area
ovulation: the release of an oocyte from a mature follicle in the ovary of a vertebrate
penis: the male reproductive structure for urine elimination and copulation
placenta: the organ that supports the transport of nutrients and waste between the mothers and fetus’ blood in eutherian mammals
progesterone: a reproductive hormone in women; assists in endometrial regrowth and inhibition of FSH and LH release
prostate gland: a structure that is a mixture of smooth muscle and glandular material and that contributes to semen
scrotum: a sac containing testes, exterior to body
semen: a fluid mixture of sperm and supporting materials
seminal vesicle: a secretory accessory gland in male; contributes to semen
seminiferous tubule: the structures within which sperm production occurs in the testes
testes: a pair of male reproductive organs
testosterone: a reproductive hormone in men that assists in sperm production and promoting secondary sexual characteristics
uterus: a female reproductive structure in which an embryo develops
vagina: a muscular tube for the passage of menstrual flow, copulation, and birth of offspring