21 Introduction to Interpretation of Lab Values
Learning Outcomes
By the end of this chapter, learners will be able to:
- explain types of units used in laboratory testing (Conventional and Standard International Units),
- explain the use of reference ranges and critical values, and
- describe factors which affect the interpretation of numerical lab results.
Units in Laboratory Testing
At times, individuals will have various laboratory (lab) tests taken to aid in monitoring their health. Generally, you will come across lab results measured in Standard International (SI) units. Conventional Units (CU) are used in some settings, particularly in the United States, and so you may come across lab values using conventional units in American learning activities or when reviewing results in a client’s chart if they were transferred from the United States. If you find yourself needing to convert between CU and SI units, there are a variety of conversion charts outlining conversion factors (CF) online. In some lab tests, the type of units used in conventional and SI systems are the same. Included in the table below are examples of differences in types of units used for some common lab tests. Do you recall what the unit abbreviations stand for? Refer back to the conversion table as needed.
| Lab Test | Example for Conventional Units | Example for Standard International Units | Conversion Factor |
|---|---|---|---|
| hemoglobin | 13.4 g/dL | 134 g/L | 10 |
| potassium, serum | 3.9 mEq/L | 3. 9 mmol/L | 1 |
| thyroxine, free | 1.1032 ng/dL | 14.2 pmol/L | 12.871 |
CU x CF = SI UnitsSI Units/CF = CU
Reference Ranges[1]
When a lab test is measuring an amount of a particular substance in the body, it is typical that normal results will vary slightly between individuals. A reference range shows a spread of possible values you would expect to find for a particular test and is usually reported alongside the results of the lab test.
Serum Potassium Reference Range
- Serum Potassium Reference Range = 3.5 to 5.0 mmol/L
- This means any value below 3.5 is considered low,
- any value above 5.0 is considered high.
- Therefore, most people have a normal value between 3.5 to 5.0 mmol/L.
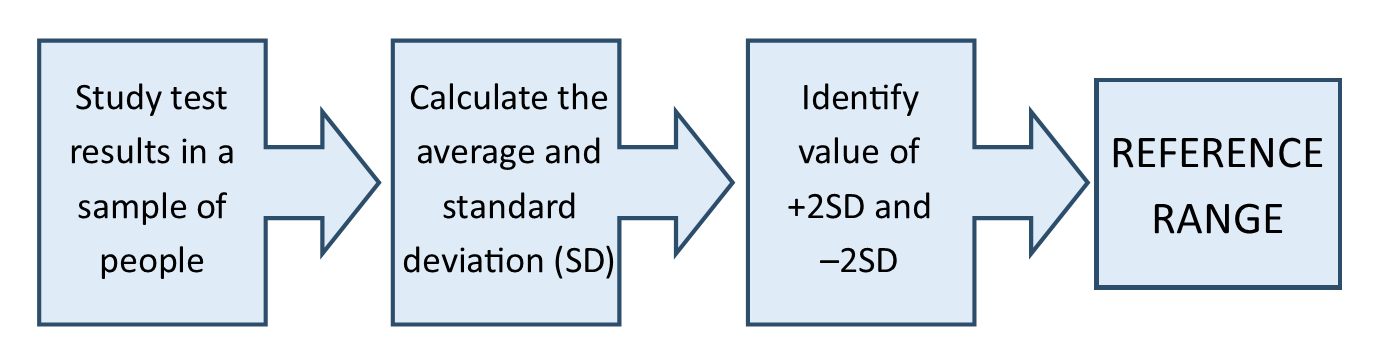
These ranges are based on the results of studies which measure the results of a particular lab test in a large number of people. Researchers identify the average result and show the distribution of possible values in a graph. They determine what the standard deviation is for a particular laboratory test and identify values for up to 3 standard deviations away from the average result. Reference ranges usually correlate to the values of 2 standard deviations below and above the average value calculated from the study. This means that some people will have a normal value slightly outside of the reference range.
It’s worth noting a study must follow best practice guidelines in order to ensure that the results are valid. For instance, the population sample used in a study should be diverse, so results are not skewed. If a researcher was trying to determine a reference range for hemoglobin and the majority of the study participants had a diagnosis of anemia, the resulting average value of hemoglobin would likely be much lower than if the study participants had a diverse distribution of characteristics which could affect the value being studied. This would not give a good representation of average hemoglobin levels.
Sometimes, there are multiple reference ranges for a particular test because characteristics like age and sex affect the amount of some substances in our bodies. Other factors which can affect laboratory results are time of day or a specific phase of a person’s menstrual cycle. The following tables show some examples where multiple reference ranges are used for a particular test.
| Age | Reference Ranges |
|---|---|
| Newborn | 4.5 to 7.2 mEq/L |
| 2 days to 3 months | 4.0 to 6.2 mEq/L |
| 3 months to 1 year | 3.7 to 5.6 mEq/L |
| 1 year to 16 years | 3.5 to 5.0 mEq/L |
| Adult | 3.5 to 5.0 mEq/L |
| Sex | Reference Ranges |
|---|---|
| Female | ≤ 2.6 nmol/L |
| Male | 6.1 to 27.1 nmol/L |
| Phase | Reference Ranges |
|---|---|
| Midfollicular Phase | 3.9 to 8.8 IU/L |
| Midcycle Peak | 4.5 to 22.5 IU/L |
| Midluteal Phase | 1.8 to 5.1 IU/L |
| Postmenopausal | 16.7 to 113.6 IU/L |
You may notice that reference ranges at particular laboratories may be reported differently from those in a diagnostic manual, as there are some factors which can affect the results of particular tests. For example, arterial blood gas (ABG) results are affected by altitude. Therefore, a laboratory in Banff, Alberta (the city with the highest altitude in Canada) may list their ABG results with a slightly different reference range that Vancouver, British Columbia (at sea level). In other cases, the way that a specific test is processed at an individual laboratory varies, and may result in slightly different test results.
| Source | Adult Female | Adult Male |
|---|---|---|
| Medical Council of Canada | 115 to 155 g/L | 125 to 170 g/L |
| Health Link BC | 120 to 160 g/L | 140 to 174 g/L |
Critical Thinking Question
- How do you access reference ranges for the clinical practice site you are working in?
Critical Values[2]
In some cases, lab test results may be reported with a warning of a critical value to help alert health care staff of serious results. Critical values always fall outside of the reference range. Results with a critical value may pose an immediate threat to a person’s wellbeing and require urgent intervention to protect health.
Depending on the test, there may only be a critical high or a critical low, or a test might have both a critical high and low. It is also possible that a particular test may not have a critical value associated with it, this often happens in cases where results are reported as positive or negative.
For instance, a pregnancy test detecting human chorionic gonadotropin (hCG) do not have a critical result. Each health care site and laboratory you work in will have a particular list of critical values they use and a policy and process for responding to critical values.
Serum Potassium Reference Range = 3.3 to 5.0 mmol/L
Critical Low < 3.0 mmol/L
Critical High > 6.1 mmol/L
Interpreting Lab Values
Reference ranges and critical values are important to understand when interpreting lab results, but they are not the only factors to be considered when determining what the result means for an individual.
Interpretation of results often requires knowledge of additional information about the individual’s health history and their care plan. In addition, conversations between members of the interdisciplinary team may be necessary in complex situations. It is also important to be mindful of considering whether or not the test results are accurate.
Here are some questions you can ask yourself to guide your critical thinking process when interpreting lab results. Please note that these questions are focused on the interpretation of numerical values of the lab results and do not encompass all of the nursing care and assessments required for patients who have abnormal lab results!
Practice exercises in this chapter are focused on individual lab tests, however in actual nursing practice you will often be interpreting results of multiple lab tests in conjunction with each other.
Questions to Guide Your Critical Thinking Process
- How does the actual result compare to the result I expected for this person?
- Did I expect the result to be positive or negative, high, low or within the reference range?
- Has the person received a recent intervention which would cause a change in this test result?
- What was the previous result of this test (if it has been done before)?
- What do I know about their current condition and their history that would tell me about why this result was obtained?
- Does this person have a health issue that would impact the result of this test?
- Does the person have assessment findings that correlate with the result of the test?
- How quickly are test results changing?
- How accurate are the test results?
- Was there anything that interfered with any part of the procedure which could impact accuracy?
- Are there any conditions which could cause a false positive or false negative for this person?
- Does this person require follow up care based on the test result?
- What is the person’s goal of care?
- What is the person’s code status?
- Does the person want or need education about the result?
- What kind of monitoring is required?
- What symptoms would I expect to see based on the result of the test?
- Has the person received new orders from the primary care provider?
- What else do I need to know to effectively care for this person?
- Do I need to connect with other members of the interprofessional team?
- What reference materials can I access to increase my understanding related to this topic?
Case Study
You are caring for a client on the second day after having a total hip arthroplasty. You are following up on the client’s daily hemoglobin test on post op day 2. Here is a sample of how you might use the following prompting questions to interpret the client’s hemoglobin result. We will use the following information to work through this example:
- Client MB, male, age 71, full code.
- No history of bleeding disorders.
- Hemoglobin results: Pre op 162 g/L, Post op day 1 125 g/L, Post op day 2 79 g/L, Reference range 125 to 170 g/L.
- Pain level 4/10, moderate shadowing to hip dressing.
- Appears somewhat pale and reports feeling tired today.
Questions
- How does the actual result compare to the result I expected for this person?
- Did I expect the result to be positive or negative, high, low or within the reference range? Considering if there was visible bleeding, how saturated the dressing was (the client had moderate shadowing to the dressing) and typical prognosis after a total hip surgery, I expected the client to have a lower value for hemoglobin today. The reference range given by the lab is 125 to 170 g/L. (If you do not see a reference range in a case study question, refer to a diagnostic and lab test manual).
- Has the person received a recent intervention which would cause a change in this test result? I would consider if they had a recent blood transfusion, what typical blood loss is like during a total hip arthroplasty.
- What was the previous result of this test (if it has been done before)? I would refer back to the previous results on the chart-I see the previous results were 162 and then 125.
- What do I know about their current condition and their history that would tell me about why this result was obtained?
- Does this person have a health issue that would impact the result of this test? Yes, they just had a major surgery.
- Does the person have assessment findings that correlate with the result of the test? I would look to see if VS had changed today (particularly drop in blood pressure or increase in heart rate). I’ll observe for skin condition (CWMS) , saturation or shadowing on the dressing and the client’s reported feeling of pain, energy levels and anxiety.
- How quickly are test results changing? Relatively quickly, there was a significant drop both days.
- How accurate are the test results?
- Was there anything that interfered with any part of the procedure which could impact accuracy? no
- Are there any conditions which could cause a false positive or false negative for this person? no
- Does this person require follow up care based on the test result?
- What is the person’s goal of care? To regain mobility post op and be discharged home. I would also need to know if they accept blood products as part of their treatment plan.
- What is the person’s code status? Full code, this indicates I anticipate treatment for low hemoglobin to be given, as warranted by specific test results.
- Does the person want or need education about the result? I would need to ask if the client understood the results given by the primary care provider and/or if they wanted further information.
- What kind of monitoring is required? VS, surgical site and dressing, client’s subjective symptoms, repeat lab work.
- What symptoms would I expect to see based on the result of the test? Potential change in skin colour, becoming paler, fatigue or weakness, possible shortness of breath or other symptoms related to reduced oxygenation to tissues.
- Has the person received new orders from the primary care provider? I would need to check the chart for further orders, anticipating a potential blood transfusion or support with intravenous fluids
- What else do I need to know to effectively care for this person?
- Do I need to connect with others members of the interprofessional team? I need to ensure the primary care physician is aware of the results, I would inform the physio or rehab assistant if they were coming in soon to assist with mobilizing the client.
- What reference materials can I access to increase my understanding related to this topic? Diagnostic test manual, articles related to blood loss and hip arthroplasty.
Sample Exercise 21.1
Critical Thinking Questions[3][4]
Key Takeaways
- Laboratory results can be reported in Conventional or Standard International Units.
- Conversion factors can be used to convert between the types of units.
- Reference ranges identify the spread of lab values when values fall in a range.
- Reference ranges for a particular test may vary between individual laboratories or for individuals with particular characteristics (eg. age, sex)
- Critical values refer to lab values which fall out of the normal reference range and are considered to be an immediate threat to health.
- Interpreting lab values requires consideration of multiple factors related to the context of the individual.
Practice Set 21.1
Practice Set 21.2
Practice Set 21.2: Interpreting urine drugs of abuse screen
A client is brought to the emergency department with decreased level of consciousness. On arrival the Glasgow coma scale was 12/15. As part of the investigations, a urine for drugs of abuse screen was taken and is positive for opiates. The client’s spouse is adamant the client does not use opiates. No other clear reason for decreased level of consciousness is apparent at this time.
Read the following questions and determine the most important factors to consider for each question.
- How does the actual result compare to the result I expected for this person?
- What do I know about their current condition and their history that would tell me about why this result was obtained?
- How accurate are the test results?
Answers:
- Were there any medications given in the ER which would impact this test result?
- A thorough history, including current prescriptions, must be taken if not already complete. If naloxone was given after the test results were received, did it have any effect on the client’s condition?
- Is it possible to have a false positive for opiates from this test? Yes, there are a variety of over the counter and prescription medications which can cause false positives.
Practice Set 21.3
Practice Set 21.3: Interpreting Arterial Blood Gases
A client is admitted to the hospital with hyperemesis gravidarum during the first trimester of pregnancy. They have vomited multiple times today despite taking antiemetics. Additional symptoms include persistent nausea, fatigue, muscle cramps, and mild disorientation. The client is started on IV fluid to rehydrate and undergoes a variety of diagnostic testing, including examination of arterial blood gases.
- pH = 7.46
- PaCO2 = 50 mmHg
- PaO2 = 97 mmHg
- HCO3- = 35 mEq/L
Use the following suggested questions to discuss the result. Make note of additional information you might need to gather when answering these questions.
- Do these results indicate a specific acid-base imbalance?
- How does the actual result compare to the result I expected for this person?
- Did I expect the result to be positive or negative, high, low or within the reference range?
- Has the person received a recent intervention which would cause a change in this test result?
- What was the previous result of this test (if it has been done before)?
- What do I know about their current condition and their history that would tell me about why this result was obtained?
- Does this person have a health issue that would impact the result of this test?
- Does the person have assessment findings that correlate with the result of the test?
- How quickly are test results changing?
- How accurate are the test results?
- Was there anything that interfered with any part of the procedure which could impact accuracy?
- Are there any conditions which could cause a false positive or false negative for this person?
- Does this person require follow up care based on the test result?
- What is the person’s goal of care?
- What is the person’s code status?
- Does the person want or need education about the result?
- What kind of monitoring is required?
- What symptoms would I expect to see based on the result of the test?
- Has the person received new orders from the primary care provider?
- What else do I need to know to effectively care for this person?
- Do I need to connect with others members of the interprofessional team?
- What reference materials can I access to increase my understanding related to this topic?
Answers:
- These results indicate the client is in a state of partially compensated metabolic alkalosis. The pH is high, therefore the client is in a state of alkalosis. Increases in carbon dioxide would shift the pH downwards and increases in bicarbonate would shift the pH upwards. This means the client is in metabolic alkalosis, since the resulting direction of change in pH of an increased bicarbonate level matches the current state of the pH. It is partially compensated as there are changes in carbon dioxide levels without the pH shifting back to a normal level.
- Excessive vomiting can lead to metabolic alkalosis in some severe cases. From the information provided, there are no interventions noted which would cause metabolic alkalosis (eg. excessive gastric suctioning). It is unknown if this patient had previous ABGs taken, and there is no past medical history noted which would affect pH balance.
- The information provided in this case indicates they had persistent, severe vomiting which is a symptom which can lead to alkalosis. Assessment findings which can be associated with metabolic alkalosis include fatigue, muscle cramps and confusion. Therefore, the patient condition correlates with the lab results.
- You may wonder if the sample result is accurate. Results may not be accurate if the test was not collected, stored or handled properly. You might wonder if it was possible that a venous blood sample was taken and not arterial. Aside from double checking with the person who drew the labs and checking to ensure the order was entered correctly you might consider how a venous sample might differ from an arterial sample. Knowing that a venous blood gas would commonly give a lower pH, slightly higher CO2 and bicarb level, it is unlikely to be a venous sample because the pH is higher that normal.
- After reviewing the abnormal ABG results, you should determine how often the client needs reassessment. This can be informed by the frequency of vomiting, the client’s current vitals signs, hospital protocols and types of treatment being provided. At minimum, the client will need to be assessed hourly while receiving intravenous fluid replacement. Check the orders to see if there is a repeat ABG ordered for a particular time or other associated lab test results, such as electrolyte levels. Treatments you should expect are fluid replacement and management of nausea and vomiting. In addition, you could be anticipating what other signs and symptoms and complications you should assess for, such as other electrolyte imbalances or signs of worsening condition, such as further changes in orientation, level of consciousness and signs of seizure activity.
- Review information about collection and interpretation of ABG’s in the hospital lab manual, your nursing textbooks, the hospital library and/or online reference materials.
- Health Link BC. (2021, December). Complete blood count. https://www.healthlinkbc.ca/tests-treatments-medications/medical-tests/complete-blood-count-cbc Medical Council of Canada. (2023). Clinical laboratory tests: Adult normal values. https://mcc.ca/objectives/normal-values/ PediaMCU: Cairo University Specialized Pediatric Hospital. (2022). Reference values for children. https://pediamcu.com/172/ ↵
- Critical Values List ARUP Laboratories National Reference Laboratory. https://www.aruplab.com/Testing-Information/resources/PDF_Brochures/ARUP_Critical_Values.pdf ↵
- Cheung, A. S., Lim, H. Y., Cook, T., Zwickl, S., Ginger, A., Chiang, C., & Zajac, J. D. (2020). Approach to interpreting common laboratory pathology tests in transgender individuals. The Journal of Clinical Endocrinology & Metabolism, (106)3, 893-901. https://doi.org/10.1210/clinem/dgaa546 ↵
- Irwig, S. M. (2021). Which reference range should we use for transgender and gender diverse patients? The Journal of Clinical Endocrinology & Metabolism, 106(3), 1479–1480. https://doi.org/10.1210/clinem/dgaa671 ↵

