6 Physical Development in the Preschool Years
Chapter Objectives
After this chapter, you should be able to:
- Describe the physical changes that occur in early childhood.
- Explain how to provide health nutrition for 3- to 5-year-olds.
- Summarize how to support the progression of motor skills with age-appropriate activities.
- Discuss sleep needs during early childhood and sleep disorders that may affect children.
- Explain the development behind toilet training and some elimination disorders that children may experience.
- Discuss risks of and a variety of ways to promote and protect children’s health and safety.
Introduction
During the early childhood years of ages three to five we see significant changes in the way children look, think, communicate, regulate their emotions, and interact with others. Children are often referred to as preschoolers during this time period. We’ll examine the physical changes of the preschooler in this chapter.
Growth in Early Childhood
Preschool aged children tend to grow about 3 inches in height each year and gain about 4 to 5 pounds in weight each year. A 3 year old is very similar to a toddler with a large head, large stomach, short arms and legs. But by the time the child comes out of this stage, their torso has lengthened, and their body proportions have become more like those of adults. According to WHO[1], the average 5 year old weighs approximately 43 pounds and is about 43 inches in height. This growth rate is slower than that of infancy.
nutritional concerns
That slower rate of growth is accompanied by a reduced appetite between the ages of 2 and 5. Children between the ages of 2 and 3 need 1,000 to 1,400 calories, while children between the ages of 4 and 8 need 1,200 to 2,000 calories [2]. This change can sometimes be surprising to parents and lead to the development of poor eating habits. However, by providing adequate, sound nutrition, and limiting sugary snacks and drinks, the caregiver can be assured that 1) the child will not starve; and 2) the child will receive adequate nutrition. Caregivers need to keep in mind that they are setting up taste preferences at this age. Young children who grow accustomed to high fat, very sweet and salty flavours may have trouble eating foods that have more subtle flavours such as fruits and vegetables. Consider the following advice about establishing eating patterns for years to come[3]. Notice that keeping mealtime pleasant, providing sound nutrition and not engaging in power struggles over food are the main goals[4].
tips for establishing healthy eating habits
- Don’t try to force your child to eat or fight over food. Of course, it is impossible to force someone to eat. But the real advice here is to avoid turning food into a power struggle so that food doesn’t become a way to gain favour with or express anger toward someone else.
- Recognize that appetite varies. Children may eat well at one meal and have no appetite at another. Rather than seeing this as a problem, it may help to realize that appetites do vary. Continue to provide good nutrition at each mealtime (even if children don’t choose to eat the occasional meal).
- Keep it pleasant. This tip is designed to help caregivers create a positive atmosphere during mealtime. Mealtimes should not be the time for arguments or expressing tensions. You do not want the child to have painful memories of mealtimes together or have nervous stomachs and problems eating and digesting food due to stress.
- No short order chefs. While it is fine to prepare foods that children enjoy, preparing a different meal for each child or family member sets up an unrealistic expectation from others. Children probably do best when they are hungry and a meal is ready. Limiting snacks rather than allowing children to “graze” continuously can help create an appetite for whatever is being served.
- Limit choices. If you give your preschool aged child choices, make sure that you give them one or two specific choices rather than asking “What would you like for lunch?” If given an open choice, children may change their minds or choose whatever their sibling does not choose!
- Serve balanced meals. Meals prepared at home tend to have better nutritional value than fast food or frozen dinners. Prepared foods tend to be higher in fat and sugar content as these ingredients enhance taste and profit margin because fresh food is often more costly and less profitable. However, preparing fresh food at home is not costly. It does, however, require more activity. Including children in meal preparation can provide a fun and memorable experience.
- Don’t bribe. Bribing a child to eat vegetables by promising dessert is not a good idea. First, the child will likely find a way to get the dessert without eating the vegetables (by whining or fidgeting, perhaps, until the caregiver gives in). Secondly, it teaches the child that some foods are better than others. Children tend to naturally enjoy a variety of foods until they are taught that some are considered less desirable than others. A child, for example, may learn the broccoli they have enjoyed is seen as yucky by others unless it’s smothered in cheese sauce! [5].

meal recommendations for preschool aged children
The Dieticians of Canada recommend that preschool aged children should be offered the same foods that the rest of the family eats. It is recommended that families/caregivers offer foods with different tastes, textures and colours according to Canada’s Food Guide [6]
Table : Sample Menu 1 for Preschoolers: 3 to 5 years old[7]
| Sample Menu 1 | |
|---|---|
| Breakfast | Mini mushroom omelettes or breakfast cups Strawberries and banana slices Milk |
| Morning Snack | Quark and berries parfait Water |
| Lunch | Cream of parsnip and carrot soup 100% whole wheat unsalted crackers or pita bread Raw vegetables (carrots, celery sticks, red pepper slides) with salad dressing for dipping Milk |
| Afternoon Snack | Apple slices with nut butter or cheddar cheese Water |
| Dinner | Mini meatballs Whole wheat pasta with tomato and vegetable pasta sauce Milk |
| Bedtime Snack | Granola and fruit bites |
Table Sample Menu 2 for Preschoolers: 3 to 5 years old[8]
| Sample Menu 2 | |
|---|---|
| Breakfast | Oatmeal pancakes with apple sauce Milk |
| Morning Snack | Yogurt and fruit smoothie |
| Lunch | Tuna grilled cheese or mini sandwiches on multigrain or whole wheat crackers Cucumber slices with dip Orange wedges Milk |
| Afternoon Snack | Hummus with raw vegetables (carrots, celery sticks, red pepper slices) baked tortilla chips or whole wheat pita bread Water |
| Dinner | Tofu vegetable stir fry with brown rice Milk |
| Bedtime Snack | Chocolate and almond bites bars |
brain maturation
Brain Weight
Brain growth slows during the preschool years. The brain is about 75% its adult weight by two years of age and by age 6, it is approximately 95% its adult weight. Myelination and the development of dendrites continues to occur in the cortex and as it does, we see a corresponding change in the child’s abilities. Significant development in the prefrontal cortex (the area of the brain behind the forehead that helps us to think, strategize, and control emotion) makes it increasingly possible to control emotional outbursts and to understand how to play games. Consider 4- or 5-year-old children and how they might approach a game of soccer. Chances are, every move would be a response to the commands of a coach standing nearby calling out, “Run this way! Now, stop. Look at the ball. Kick the ball!” And when the child is not being told what to do, he or she is likely to be looking at the clover on the ground or a dog on the other side of the fence! Understanding the game, thinking ahead, coordinating movement, and handling losing improve with practice and myelination [9].
Visual Pathways
Children’s drawings are representative of the development of visual pathways; as children’s brains mature the images in their drawings change. Early scribbles and dots illustrate the use of simple motor skills. No real connection is made between an image being visualized and what is created on paper.
At age 3, the child begins to draw wispy creatures with heads and not much other detail. Gradually pictures begin to have more detail and incorporate more parts of the body. Arm buds become arms and faces take on noses, lips and eventually eyelashes.


Growth in the Hemispheres and Corpus Callosum
Between ages 3 and 6, the left hemisphere of the brain grows dramatically. This side of the brain or hemisphere is typically involved in language skills. The right hemisphere continues to grow throughout early childhood and is involved in tasks that require spatial skills such as recognizing shapes and patterns. The corpus callosum which connects the two hemispheres of the brain undergoes a growth spurt between ages 3 and 6 and results in improved coordination between right and left hemisphere tasks.
Motor Skill Development
Early childhood is a time when children are especially attracted to motion and song. Days are filled with jumping, running, swinging and clapping and every place becomes a playground. Even the booth at a restaurant affords the opportunity to slide around in the seat or disappear underneath and imagine being a sea creature in a cave! Of course, this can be frustrating to a caregiver, but it’s the business of early childhood.
Gross Motor Skills
Children continue to improve their gross motor skills as they run and jump. They frequently ask their caregivers to “look at me” while they hop or roll down a hill. Children’s songs are often accompanied by arm and leg movements or cues to turn around or move from left to right.
Gross Motor Milestones
The Continuum of Development shares that during the preschool years the development of gross motor skills focus on increasing in coordination, speed, and endurance [10]. Specifically, the following motor movements are being refined[11]:
- Walking: beginning to walk with opposite leg-arm swing, walking up stairs with alternating feet, walking down stairs with alternating feet;
- Jumping: jumping increases in co-ordination;
- Hopping: hopping on one foot increases;
- Galloping: galloping and one-foot skipping emerge;
- Throwing: throwing with rigid movements and throwing with increased co-ordination;
- Riding: pedaling and steering riding toys, and riding a tricycle smoothly;
- Movement and Expression: increasing control over own movements skills, becoming expressive using movement, expressing moods in movement, moving to music, matching movements to the rhyme and mood of the music, making patterns while moving to music, working together in shared dance and movement activities.
Indigenous Perspectives

Indigenous children love to dance with or without their Regalia (outfits). Their spirit soars when they dance. It gives them a sense of belonging and connects them to mother earth. It also reinforces what the Continuum of Development says [the development of gross motor skills focuses on increasing coordination, speed, and endurance]. As they have been watching the adults dance, young children’s dance movements really improve at this age.
Activities to Support Gross Motor Skills
Here are some activities focused on play that young children enjoy and that support their gross motor skill development.
- Tricycle
- Slides
- Swings
- Sit-n-Spin
- Mini trampoline
- Bowling pins (can use plastic soda bottles also)
- Tent (try throwing blankets over chairs and other furniture to make a fort)
- Playground ladders
- Suspension bridge on playground
- Tunnels (try throwing a bean bag chair underneath for greater challenge)
- Ball play (kick, throw, catch)
- Simon Says
- Target games with bean bags, ball, etc.
- Dancing/moving to music
- Pushing self on scooter or skateboard while on stomach

fine motor skills
Fine motor skills are also being refined as they continue to develop more dexterity, strength, and endurance. Fine motor skills are very important as they are foundational to self-help skills and later academic abilities (such as writing).
Fine Motor milestones
The Continuum of Development shares that during the preschool years the development of fine motor skills focus on the following[12]:
- Dressing: mastering simple items of clothing; dressing without assistance.
- Eating: eating using forks and knives.
- Tool Use: stringing large beads, cutting paper with scissors, cutting a straight line.
- Drawing: copying straight lines, copying triangles and crosses.
activities to support fine motor skills
Here are some fun activities that will help children continue to refine their fine motor abilities. Fine motor skills are slower to develop than gross motor skills, so it is important to have age-appropriate expectations and play-based activities for children.
- Pouring water into a container
- Drawing and colouring
- Using scissors
- Finger painting
- Fingerplays and songs (such as the Itsy, Bitsy Spider)
- Play dough
- Lacing and beading
- Practicing with large tweezers, tongs, and eye droppers

sleep and early childhood
Along with food and water, sleep is one of the human body’s most important physiological needs—we cannot live without it. Extended sleeplessness (i.e., lack of sleep for longer than a few days) has severe psychological and physical effects. Research on rats has found that a week of no sleep leads to loss of immune function, and two weeks of no sleep leads to death. Recently, neuroscientists have learned that at least one vital function of sleep is related to learning and memory. New findings suggest that sleep plays a critical role in flagging and storing important memories, both intellectual and physical, and perhaps in making subtle connections that were invisible during waking hours [13].
How much sleep do we need?
The amount of sleep an individual needs varies depending on multiple factors including age, physical condition, psychological condition, and energy exertion. Just like any other human characteristic, the amount of sleep people need to function best differs among individuals, even those of the same age and gender.
Though there is no magic sleep number, there are general rules for how much sleep certain age groups need. According to The Hospital for Sick Children [14]in Toronto, during the preschool years, children are sleeping approximately 10-12 hours each day, with most of the sleep occurring in one large chunk at night. This change in sleep patterns means that daytime naps will be dropped organically or weaned in order to make room for that important nighttime sleep. This may be a challenging time for children and their families as they respond to the transition. Some children may struggle to remain awake during the latter part of the day and may need extra support to regulate their behaviours and emotions during this stressful period. If the child attends a full day child care program, it is essential that the family and the educators work together to develop a sleep strategy designed in the best interest of the child.

sleepwalking (Somnambulism)
Sleepwalking (sometimes called sleepwalking disorder, somnambulism, or noctambulation) causes a person to get up and walk during the early hours of sleep. The person may sit up and look awake (though they’re actually asleep), get up and walk around, move items, or dress or undress themselves. They will have a blank stare and still be able to perform complex tasks. Some individuals also talk while in their sleep, saying meaningless words and even having arguments with people who are not there. A person who sleepwalks will be confused upon waking up and may also experience anxiety and fatigue.
According to Healthline[15], sleepwalking is most common in children aged 4-8. Most children who sleepwalk begin to do so an hour or two after falling asleep and episodes usually last from five to 15 minutes. This behaviour is typically harmless, and most children grow out of it. However, it can be dangerous if left unaddressed. It’s important to protect your child from possible injury from sleepwalking by gently guiding them back to bed once discovered. Do not try to wake the sleepwalker, as this could aggravate them. Instead, simply reassure the child with words and help steer them back to bed.
Night Terrors and Nightmare Disorder
Night terrors are characterized by a sudden arousal from deep sleep with a scream or cry, accompanied by some behavioural manifestations of intense fear. They are often accompanied by sleep walking. Night terrors typically occur in the first few hours of sleep, during stage 3 NREM sleep and tend to happen during periods of arousal from delta sleep (i.e., slow-wave sleep). According to the Hospital for Sick Children [16], unlike nightmares, children who have night terrors rarely wake up during the episode. They often do not have memories of the night terror. During the episode, they will show signs of fear, anxiety and general disturbance. Children are typically not fully conscious and may speak without making sense. Night terrors are common in children younger than six years old.
Toilet Training (or Toilet Learning)
Learning how to use the toilet typically occurs between the ages of 2-4. Some children show interest by age 2, but others may not be ready until months later. The average age for girls to be toilet trained is 29 months and for boys it is 31 months, and 98% of children are trained by 36 months [17]. The child’s age is not as important as his/her physical, emotional and cognitive readiness. If started too early, it might take longer to support a child in learning how to use the toilet.
According to the Canadian Paediatric Society via Caring for Kids (2018), caregivers can assume that a child is ready for toilet learning when they:
- Show an interest in the potty (by watching you, or by liking books about learning to use the potty).
- Are dry in their diaper for several hours in a row.
- Have regular and predictable bowel movements or knows when they are urinating or having a bowel movement. For example, child might go into another room or hide behind furniture.
- Are steady and balanced when sitting on the toilet or potty.
- Can follow one or two simple instructions.
- Can let you know when they need to use the potty.
- Want to be independent.
If a child resists being trained or it is not successful after a few weeks, it is best to take a break and try again when they show more significant interest in the process. Most children master daytime bladder control first, typically within two to three months of consistent toilet training. However, nap and nighttime training might take months or even years.

Elimination Disorders
Some children experience elimination disorders including:
- enuresis – the repeated voiding of urine into bed or clothes (involuntary or intentional) after age 5
- encopresis – the repeated passage of feces into inappropriate places (involuntary or intentional).
The prevalence of enuresis is 5%-10% for 5 year-olds, 3%-5% for 10 year-olds and approximately 1% for those 15 years of age or older. Around 1% of 5 year-olds have encopresis, and it is more common in males than females. These are diagnosed by a medical professional and may require treatment [18].
Health in early childhood
childhood obesity
Childhood obesity is a complex health issue. It is diagnosed when a child is well above the normal or healthy weight for his or her age and height. Childhood obesity is on the rise; obesity rates among children and youth in Canada have nearly tripled in the last 30 years [19]. Where people live can affect their ability to make healthy choices. Obesity disproportionally affects children from low-income families.
causes of obesity
The causes of excess weight gain in young people are similar to those in adults, including factors such as a person’s behaviour and genetics. Behaviours that influence excess weight gain include:
- eating high calorie, low-nutrient foods
- not getting enough physical exercise
- sedentary activities (such as watching television or other screen devices)
- medication use
- sleep routines

consequences of obesity
The consequences of childhood obesity are both immediate and long term. It can affect physical as well as social and emotional well-being.
More immediate Health Risks:
- High blood pressure and high cholesterol, which are risk factors for cardiovascular disease (CVD).
- Increased risk of impaired glucose tolerance, insulin resistance, and type 2 diabetes.
- breathing challenges, such as asthma and sleep apnea.
- Joint problems and musculoskeletal discomfort.
- Fatty liver disease, gallstones, and gastro-esophageal reflux (i.e., heartburn).
Childhood Obesity is also related to:
- Psychological challenges, such as anxiety and depression.
- Low self-esteem and lower self-reported quality of life.
- Social problems such as bullying and stigma.
Future Health Risks:
- Children who have obesity are more likely to become adults with obesity. Adult obesity is associated with increased risk of a number of serious health conditions including heart disease, type 2 diabetes, and cancer.
- If children have obesity, their obesity and disease risk factors in adulthood are likely to be more severe.
To fight off the risk of obesity in preschool aged children, the Government of Canada [20] suggests that caregivers support children in developing healthy eating habits and encourage physical activity. They suggest the following:
Tips for developing healthy eating habits:
- Use the Canada Food Guide to plan meals/snacks.
- Set a good example by being a role model for healthy eating. Children are more likely to try new foods if you eat them too.
- Limit distracted eating by keeping the food at the meal the focus.
- Involve children in planning and preparing meals and snacks.
Tips for encouraging physical activity:
- Aim for at least 180 minutes spent in a variety of physical activities spread throughout the day, including at least 60 minutes of energetic play [21].
- Set a good example by being a role model for participating in consistent physical activity.
- Limit the amount of time your children spend on sedentary activities like watching television, playing video games, and surfing the web.
food allergies
According to Food Allergy Canada [22],
- more than 3 million Canadians self-report having at least one food allergy.
- almost 500,000 Canadian children under 18 years have food allergies.
- peanut allergies in Canada affect about 2 in 100 children.
A food allergy occurs when the body has a specific and reproducible immune response to certain foods. Although the immune system normally protects people from germs, in people with food allergies, the immune system mistakenly responds to food as if it were harmful. The body’s immune response can be mild, moderate, severe or life-threatening. An example of a severe or life-threatening response would be anaphylaxis. Anaphylaxis is a sudden and severe allergic reaction that may cause death. Children at risk of anaphylaxis will likely have immediate access to an epinephrine auto-injector (e.g. EpiPen®, ALLERJECT®) which contains life-saving medication to treat an allergic reaction. Under Sabrina’s Law, every school board in Ontario is required to establish and maintain an anaphylactic policy. The law also requires schools to create individual plans for each child at risk of anaphylaxis.
Symptoms of anaphylaxis generally include two or more of these body systems[23].
- Skin: hives, swelling (face, lips, tongue), itching, warmth, redness
- Respiratory (breathing): coughing, wheezing, shortness of breath, chest pain/tightness, throat tightness, hoarse voice, nasal congestion or hay fever-like symptoms (runny itchy nose and watery eyes, sneezing), trouble swallowing
- Gastrointestinal (stomach): nausea, pain/cramps, vomiting, diarrhea
- Cardiovascular (heart): paler than normal skin colour/blue colour, weak pulse, passing out, dizziness or lightheadedness, shock
- Other: anxiety, sense of doom (the feeling that something bad is about to happen), headache, uterine cramps, metallic taste
Some preschool children may not have diagnosed food allergies, rather suffer from food intolerances. A food intolerance is the inability to digest or absorb certain foods. For example, someone with lactose intolerance doesn’t have enough of the enzyme lactase to break down the sugar (lactose) in dairy products. The symptoms of food intolerance affect the gastrointestinal tract and can cause discomfort but are generally not life-threatening[24].
Indigenous Perspectives
Poverty and the lack of access to healthy foods affect all remote Indigenous communities in Canada. Healthy foods are so expensive that poor families cannot afford it. The following link opens a paper on Tackling Poverty in Indigenous Communities in Canada The following blog The Challenge of Feeding the North discusses food insecurity in remote communities in Canada This is a problem that has been at the forefront since Indigenous people have been placed on reservations.
oral health
According to the Ontario Dental Hygienist’s Association [25], teeth are an integral part of overall health and with proper care people can keep their teeth for a lifetime. Preschool aged children should be encouraged to build healthy eating habits to protect their teeth and encouraged to brush their teeth twice a day. When teeth are not well taken care of, children can suffer from oral infections and early childhood cavities (ECC). ECC is a severe form of tooth decay in the primary teeth of infants and toddlers. It affects more than 10% of preschool-age children in Canada. ECC can be caused by passing bacteria from the parent/caregiver to the child (e.g., through kisses, sharing toothbrushes, food and utensils), the amount of sugar and starches in the diet, and the time and frequency of feedings.
Tips to support positive oral care in preschool aged children:
- At this stage caregivers should still need to supervise and help children brush and floss properly. The parent can check after the child has brushed.
- The best way to check the child’s mouth after brushing is to stand behind the child so that both are facing the mirror. Lift the lip to assess the gums and the back teeth.
- Toothpaste with fluoride should only be used when the child can rinse and spit properly because swallowing toothpaste with fluoride can permanently stain a child’s adult teeth. Use only a small amount of toothpaste (pea-size or smaller).
- Encourage regular brushing and flossing as the child gets older.

protection from illness
Two important ways to help protect children from illness are immunization and hand-washing.
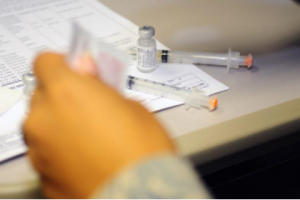
Immunizations
While vaccines begin in infancy, it is important for children to receive additional doses of vaccines to keep them protected. These boosters, given during the preschool years, are doses of the vaccines they received earlier in life to help them maintain the best protection against vaccine-preventable diseases.
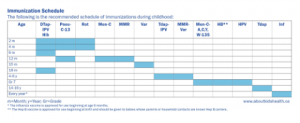
The following chart shows the recommended schedule of immunizations during childhood for the province of Ontario as of December 2016. For the most current recommendations according to the National Advisory Committee on Immunization and for each province and territory go to the Government of Canada website.
The Province of Ontario [26], shares in the Child Care and Early Years Act, 2014 that families are to provide proof of immunization (or appropriate exemption documents) for certain diseases if their child attends a licensed childcare centre in Ontario. A child may be exempt from immunization requirements for medical reasons, philosophical reasons or religious reasons. It should be noted that children who are not vaccinated are at increased risk of disease and may be removed from the child care centre during a disease outbreak [27].
Hand-Washing
Hand-washing is one of the best ways to prevent the spread of illness. It’s important for children (and adults) to wash their hands often, especially when they are likely to get and spread germs, including:
- Before, during, and after preparing food.
- Before eating food.
- After blowing nose, coughing, or sneezing.
- After using the toilet.
- After touching an animal, animal feed, or animal waste.
- After touching garbage.
It’s important for children to learn how to properly wash their hands. When washing hands children (and adults) should follow these five steps every time.
1. Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap.
2. Lather your hands by rubbing them together with the soap. Lather the backs of your hands, between your fingers, and under your nails.
3. Scrub your hands for at least 20 seconds. Need a timer? Hum or sing the Happy Birthday song or ABCs from beginning to end twice.
4. Rinse your hands well under clean, running water.
5. Dry your hands using a clean towel or air dry them [28]

Caregivers can help keep children healthy by:
- Teaching them good hand-washing techniques.
- Reminding their kids to wash their hands.
- Washing their own hands with the children [29].
safety
Childhood injury is defined as “the physical damage that results when a human body is subjected to energy that exceeds the threshold of physiological tolerance or results in lack of one or more vital elements, such as oxygen” [30].
Through statistics shared via the Canadian Pediatric Society [31],
- In Canada, injury is the leading cause of death for not only children, but for all Canadians between the ages of one and 44.
- Between 1994 and 2003, approximately 390 Canadian children age 14 years and under died from unintentional injuries annually, while another 25,500 were hospitalized.
- In 2004, injuries to Canadians cost $19.8 billion in health care costs and lost productivity, of which $16.0 billion resulted from unintentional causes. Of this, almost $3 billion could be accounted for by falls and transport-related injuries to children and youth from birth to 19 years of age.
The most common causes of injury in preschool aged children are due to the following[32]:
- Falls: Falls are the leading cause of injury in preschool aged children. Examples of how falls can occur are as follows: on the stairs and steps, off furniture, by slipping, tripping and stumbling, by using furniture to climb out windows or balconies, by not using age appropriate playground equipment, and/or on hard surfaces.
- Choking, strangulation and suffocation are leading causes of injury-related deaths for children in Canada. Children can be harmed by: choking on food and small objects, strangling from items such as ropes, blind cords, or draw strings in clothing, suffocating in cribs or beds, being left in a car.
- Burns: A child’s skin burns four times faster and deeper than an adult’s at the same temperature. Common causes of burns include: scalds from steam, hot water, tipped-over coffee cups, hot foods or cooking fluids, contact with flames or other hot objects such as curling iron or fireplace, chemical burns from items such as batteries or bleach, electrical burns from biting on electrical cords or sticking fingers or objects into outlets, too much exposure to the sun.
- Poisoning: Half of all poison exposures happen to children under five years of age. Common poisonous products: medications, household cleaners, alcohol, plants, fertilizers, pesticides, paint thinner, antifreeze, carbon monoxide
- Drowning or near drowning: All children are at risk for drowning but children under age five have a higher risk. It can happen quickly and silently in only a few centimetres of water.
Childhood injuries are preventable. It is important for caregivers to consistently and thoroughly supervise young children.

Summary
- The physical characteristics of preschoolers.
- Healthy nutrition.
- The changes in the brain.
- The progression of motor skills and developmentally appropriate ways to support that development.
- Sleep and sleep disorders.
- Toilet training and elimination disorders.
- And ways to keep children healthy and safe.
Attribution
This chapter is copied from Chapter 9 in Child Growth and Development Canadian Ed by Tanya Pye; Susan Scoffin; Janice Quade; and Jane Krieg , and shared under a CC-BY-NC-SA 4.0 license.
- World Health Organization. (2021). Weight for age (5-10 years). Retrieved from https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/weight-for-age-5to10-years, ↵
- Mayo Clinic, 2016a, as cited in Paris, Ricardo, Raymond, & Johnson, 2021 ↵
- Rice, 1997, as cited in Paris, Ricardo, Raymond, & Johnson, 2021 ↵
- Leon, A. (n.d.). Children’s development: Prenatal through adolescent development. Retrieved from https://docs.google.com/document/d/1k1xtrXy6j9_NAqZdGv8nBn_I6-lDtEgEFf7skHjvE-Y/edit ↵
- Ibid. ↵
- Dieticians of Canada. (2020). Sample meal plan for feeding your preschooler (Ages 3 to 5). Retrieved from https://www.unlockfood.ca/en/Articles/Childrens-Nutrition/Cooking-and-Meal-Planning/Sample-meal-plan-for-feeding-your-preschooler-(age ↵
- Ibid. ↵
- Ibid. ↵
- Lumen Learning. (n.d.). Physical development. In Lifespan development. Retrieved from https://courses.lumenlearning.com/lifespandevelopment2/chapter/physical-development-during-early-childhood/ ↵
- Ontario Ministry of Education. (2014). Exerpts from “ELECT”. Retrieved from https://countrycasa.ca/images/ExcerptsFromELECT.pdf ↵
- Ibid. ↵
- Ibid. ↵
- Leon, A. (n.d.). Children’s development: Prenatal through adolescent development. Retrieved from https://docs.google.com/document/d/1k1xtrXy6j9_NAqZdGv8nBn_I6-lDtEgEFf7skHjvE-Y/edit ↵
- SickKids. (2020). Sleep: Benefits and recommended amounts. Retrieved from https://www.aboutkidshealth.ca/article?contentid=645&language=english ↵
- Healthline. (2018). Pediatric sleepwalking. Retrieved from https://www.healthline.com/health/sleep/sleepwalking-and-children ↵
- SickKids. (2011). Sleep terrors. Retrieved from https://www.aboutkidshealth.ca/Article?contentid=305&language=English ↵
- Boyse & Fitzgerald, 2010, as cited in Paris, Ricardo, Raymond, & Johnson, 2021 ↵
- Lally, M. & Valentine-French, S. (2019). Lifespan development: A psychological perspective (2nd ed.). Retrieved from http://dept.clcillinois.edu/psy/LifespanDevelopment.pdf ↵
- Government of Canada. (2019). Childhood obseity. Retrieved from https://www.canada.ca/en/public-health/services/childhood-obesity/childhood-obesity.html ↵
- Ibid. ↵
- CSEP. (2021). Canadian 24 hour movement guidelines for the early years. Retrieved from https://csepguidelines.ca/early-years-0-4/ ↵
- Food Allergy Canada. (2021). Food allergy FAQ’s. Retrieved from https://foodallergycanada.ca/food-allergy-basics/food-allergies-101/food-allergy-faqs/ ↵
- Food Allergy Canada. (2021). Food allergy FAQ’s. Retrieved from https://foodallergycanada.ca/food-allergy-basics/food-allergies-101/food-allergy-faqs/ ↵
- Ibid ↵
- Ontario Dental Hygenists Association. (n.d.). Dental hygiene facts: Oral care for children. Retrieved from https://odha.on.ca/wp-content/uploads/2016/08/ODHA-Facts-children.v2.pdf ↵
- Province of Ontario. (2014). Child care and early years act 2014, O. Reg. 137/15: General. Retrieved from https://www.ontario.ca/laws/regulation/150137 ↵
- Eastern Ontario Health Unit. (2021). Immunization requirements for children in licensed child care centres (Daycare). Retrieved from https://eohu.ca/en/my-community/immunization-requirements-for-children-in-licensed-child-care-centres-daycare ↵
- Centres for Disease Control and Prevention. (2021). When and how to wash our hands. Retrieved from https://www.cdc.gov/handwashing/when-how-handwashing.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Ffeatures%2Fhandwashing%2Findex.html ↵
- Centres for Disease Control and Prevention. (2020). Handwashing: A family activity. Retrieved from https://www.cdc.gov/handwashing/handwashing-family.html ↵
- Canadian Pediatric Society. (2020). Child and youth injury prevention: A public health approach. Retrieved from https://www.cps.ca/documents/position/child-and-youth-injury-prevention ↵
- Ibid ↵
- City of Toronto. (2021). Common childhood injuries. Retrieved from https://www.toronto.ca/community-people/public-safety-alerts/safety-tips-prevention/home-high-rise-school-workplace-safety/child-safety/common-childhood-injuries/ ↵

