6. QSE Process Management: Statistical Quality Control
The most common set of rules that are used to decide if QC results are acceptable are the Westgard Rules. These rules, or some variation thereof, are used in most labs in Nova Scotia to evaluate statistical qc results.
The most commonly used of the Westgard Rules include the following:
- 1 point is outside 2SD
If 1 point is outside 2SD, then reject when:
- 1 point is outside 3SD
- 2 consecutive points are outside 2SD on the same side of the mean
- Range of 2 points is greater than 4SD
- 4 Consecutive points exceed 1 SD on the same side of the mean
- 10 consecutive points are above or below the mean
You have learned about quality in all your discipline specific courses so by now you should be able to apply the qc rules for each different type of testing.
Statistical Tools
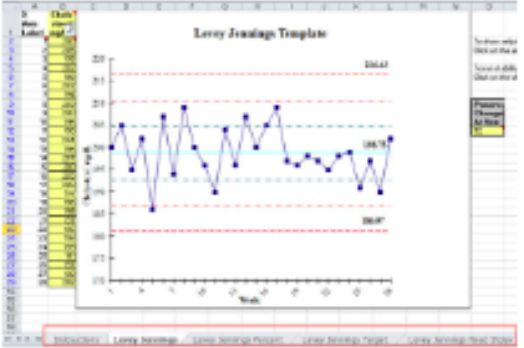
It is equally important to understand how statistical analysis of the qc results are applied to laboratory testing. There are several tools that you must know and be able to identify when you are performing qc evaluations. One of the most common control charts used in the clinical laboratory is the Levey-Jennings chart – A commonly used control chart in which individual control measurements are plotted directly on a control chart with limit lines drawn either as mean +/-2s or mean+/-3s.(Westgard). These charts are commonly used to plot and analyze the data from control results on routine Chemistry analyzers.
Other common tools that can be used to evaluate quality control statistics to ensure that the QC sample is working accurately and precisely include histograms, scatter plots and run charts. They may be used alone or in combination with other tools.
The last major requirement that must be addressed in Process Management is Change Management. Since any QMS requires that processes are constantly being reviewed and improved, the need for good change management processes is essential. According to CLSI, “the laboratory needs to evaluate and record the outcomes of control processes for opportunities to change and improve established work processes” (p.54). There are several defined processes required to successfully implement change within the laboratory.
- Processes for the identification and assessment of the reason for a change to be undertaken
- Processes for the planning and implementation of the change
- Processes for making sure that the necessary approvals are obtained before undertaking the change
- Processes to validate the effectiveness of the change
- Processes to pilot the change before it is formally accepted
- Processes for ongoing monitoring of the change to determine future adjustments and changes that may need to be addressed
- Finally, processes for staff training and competency assessment must be developed and implemented
Strong leadership has an essential ingredient in making change effectively. A culture of continuous improvement is a cornerstone of effective change management and leaders must support an environment for innovation that allows employees to bring forth suggestions for improvement and to have their contributions recognized. Because any change within the laboratory may be perceived as a threat to some staff, it is wise to implement change carefully, to make sure that everyone is aware that the change is occurring, and that everyone has been told why the change is necessary and beneficial. It is important to recognize that change is inevitable but that it usually encounters resistance.
Exercise: Process Control Scenarios
- After performing daily quality control on the CX7, the technologist observes a 41s violation for the glucose parameter. What type of error is this?
- The technologist observes that the 3.2% sodium citrate tube for a PT and APTT is only two-thirds full. What effect will this have on the patient’s coagulation results?
- As a technologist is finishing a blood draw on a heparinized tube, the nurse manager comes into the patient room to ask a question about performing a capillary draw. The technologist puts down the blood and describes to her, while showing her the correct area of the finger to use. What effect will this have on the blood in the vacutainer?
- When a technologist is evaluating the quality control from a run of phenytoin, he notices that both controls run had results outside 2SD above the mean. What should he do?
- When performing the H&E staining procedure in Histology, the technologist notices that the slides all appear very dark. How could this impact the ability to read the slide?
- The Microbiology refrigerator containing culture media malfunctioned overnight and the temperature dropped to -8 degrees before the technologist noticed that the alarm had been beeping steadily for quite awhile. What effect would this have on the plates? What effects would it have on the services of the department?
Case Study – Sample Labelling
You receive a specimen in the laboratory with a request for a complete urinalysis. The cup is labeled and you begin your testing. You finish the testing and report the results to the nursing unit. Several minutes later, you receive a telephone call from the unit telling you that the urine was reported on the wrong patient. You are told that the cup was labeled incorrectly before it was brought to the lab.
- What is the problem in this case and where did it occur?
- Would your laboratory’s QC system be able to detect or prevent this type of problem? How?
Case Study – Interdepartmental Communication
You are having a problem with the medical intensive care unit and the arterial blood gas specimens they submit to the laboratory. In the past 3 weeks, you have refused to perform blood gases on six different specimens because of small clots found in the specimens. The MICU is furious with the rejection policy, yet you believe the results would be incorrect if these specimens were used.
- Outline where the problem lies.
- What can be done to remedy this problem?
- Why would your QC system not detect this sort of error?
Case Study – Blood Draw Fails Delta Check
It was very busy day in the In-patient Blood Collection services since 2 phlebotomists were out on sick leave. An order came from the 4th floor for a timed draw. Joe, a phlebotomist from the casual pool, was still there even though his shift had ended 2 hours earlier. No one was available to collect the specimen except Joe. Knowing how important it was, he decided to go and collect the specimen before he left for the day.
When he arrived in the room, the patient was sitting on a chair between the 2 beds. Joe asked the patient for his name and to tell him which bed was his. The patient gave him the correct last name and pointed to the right bed. Joe collected the specimen from him and took it to the Nursing station where he labelled the tube as he was completing the desk clipboard.
When a second specimen was done on the same patient later in the morning, it failed the delta check. Another specimen was drawn and run and the results showed that Joe had drawn the specimen that was in error.
Questions
- What is a delta check?
- What events from this scenario could have caused the discrepancy to occur?
- What should Joe have done differently?
