25 Food and Nutrition
Learning Objectives
After reading this chapter you will:
- Be familiar with the standards for food and nutrition in regulated child care settings in Nova Scotia.
- Understand that the requirements are defined in the Government of Nova Scotia’s Standards for Food and Nutrition in Regulated Child Care Settings .
The Standards for Food and Nutrition in Regulated Child Care Settings identify the expectations for the provision of food and nutrition practices in regulated child care settings. Compliance with each of the standards is required by all child care facilities and approved family day care homes as per Regulations 25 and 26 in the Day Care Regulations.
Definitions
Agency means a person licensed to manage a family home day care program.
Care provider means a person who is approved by an agency to provide a family home day care program in the person’s home.
Facility Director means a person who provides daily onsite supervision of a facility.
Family home day program means a day care program that is provided by a care provider in the care provider’s home.
Food allergy means a sensitivity caused by a reaction of the body’s immune system to specific proteins in a food. Food allergies are estimated to affect as many as 6% of young children and 3% to 4% of adults.*
Food and Beverage Criteria means the Food and Beverage Criteria for Regulated Child Care Settings in Nova Scotia, which are based upon Eating Well with Canada’s Food Guide (Health Canada, 2007). These criteria provide specific information for choosing food and beverages, based on sodium, sugar, fibre and fat content.
Food intolerance means a food sensitivity that does not involve the individual’s immune system. Unlike food allergies, or chemical sensitivities, where a small amount of food can cause a reaction, it generally takes a more normal sized portion to produce symptoms of a food intolerance. While the symptoms of food intolerance vary and can be mistaken for those of a food allergy, food intolerances are more likely to originate in the gastrointestinal system and are usually caused by an inability to digest or absorb certain foods, or components of those foods.*
Food sensitivity means an adverse reaction to a food that other people can safely eat, and includes food allergies, food intolerances, and chemical sensitivities.
Full-day program means a day care program that is not a family home day care program and that
(i) provides day care for children who are not attending school, and
(ii) is operated for more than 4 consecutive hours per day or more than 30 hours per week.
Infant means a child who is younger than 18 months old.
Infant Feeding Plan means a written document for parents and staff/care providers to use in order to ensure that the infant’s daily nutritional needs are met. The Infant Feeding Plan will document any plans for the introduction of new foods. The Infant Feeding Plan will have a space for parents to provide comments and observations. The Infant Feeding Plan is a key communication tool for parents/guardians and staff/care providers.
Licensee means the person in whose name a license has been issued under the Act.
Part-day program means a day care program that is not a family home day care program and that
(i) provides day care for children who are older than 30 months and are not attending school, and
(ii) is operated for fewer than 4 consecutive hours per day or fewer than 30 hours per week;
Potable drinking water means water that is suitable for human consumption.
Regulated child care settings means the facility or home in which full-day, part-day, school-age and family home day care programs are offered.
Special dietary considerations means food allergies, food intolerances and food restrictions that may be related to a child’s ability to self feed, medical conditions and/or religious or cultural beliefs.
Standards for Food and Nutrition mean requirements that must be met in order to comply with Section 25(1) of the Day Care Regulations.
Staff means paid employees of a licensee and does not include care providers.
Objectives
These standards will accomplish the following:
- Enable licensees to comply with Regulations 25 and 27 in the Day Care Regulations.
- Support licensees, staff and care providers to develop menus for snacks and meals that will meet the nutritional needs of all children.
- Support licensees, staff and care providers to develop menus and make menu substitutions that reflect the healthy foods enjoyed by all children and staff in the facility or approved family day care home, as well as the kinds of foods that are easily accessible in the community, such as locally grown and produced products.
- Support licensees, staff and care providers in creating an environment that supports all children in developing healthy eating patterns and behaviours.
- Support licensees, staff and care providers in creating an environment that is inclusive and supportive of children with special dietary considerations.
- Support licensees, staff and care providers to develop a culture that fosters healthy development by promoting nutritious food and beverage choices that are consistent with the Food and Beverage Criteria for Regulated Child Care Settings in all program areas.
- Provide a framework for Public Health Nutritionists, Early Childhood Development Consultants, Licensing Officers, licensees, care providers, and staff to build capacity and understanding of healthy eating and healthy child development within regulated child care settings.
- Provide parents, families, food service providers, and the child care sector with a shared understanding of expectations for food and nutrition practices in regulated child care settings.
Scope
These standards apply to all child care settings that are regulated under the Day Care Act and Regulations. This includes licensed child care facilities and family day care homes that are approved by a licensed Family Home Day Care Agency.
These standards reflect local, national, and international food and nutrition policies and are grounded in health sciences and early human development evidence. These standards also reflect local insight and practices with respect to the provision of healthy foods in regulated child care settings. Each standard is preceded by a rationale that explains why the requirement is included.
It is the responsibility of the licensee to ensure that the standards are implemented in regulated child care settings. These standards must be followed in order to comply with requirements for the provision of food under the Day Care Regulations.
Standards must be followed in each of the following areas:
- Food and Beverages Served
- Clean Drinking Water
- Breastfeeding
- Adapting the Menu for Infants
- Food Safety
- Special Dietary Considerations
- Meal and Snack Routines
- Meal and Snack Time Environment
- Modelling Positive Attitudes Towards Food and Nutrition
- Fundraising with Food and Beverages
- Food is Not Used to Reinforce Desired Behaviours
- Special Functions
- Promotion and Advertising
Accountability and Monitoring
- The Departments of Education and Early Childhood Development and Health and Wellness and Public Health Services will review these standards, tools, and resources on an as-needed basis.
- The Departments of Education and Early Childhood Development and Health and Wellness will work with Public Health Nutritionists and partners in the nutrition and early childhood sectors to enhance pre-service and in-service training opportunities related to food and nutrition in early childhood and the requirements under these standards.
- Licensees will ensure that parents, staff, children (as appropriate), food service providers and community partners are informed of the standards and able to access them.
- The Department of Education and Early Childhood Development, Licensing Division, will monitor compliance with the Standards for Food and Nutrition in Regulated Child Care Settings through the licensing inspection process.
Evaluation
The Departments of Education and Early Childhood Development and Health and Wellness and Public Health Services will work with licensees to evaluate and improve upon the effectiveness of the standards.
1.0 Food and Beverages Served
The selection of food and beverages served in regulated child care settings is based on Eating Well with Canada’s Food Guide and complies with the Food and Beverage Criteria for Regulated Child Care Settings. Eating Well with Canada’s Food Guide outlines recommendations for a pattern of eating that supports healthy growth and development for children who are two years of age and older.
For children between the ages of six months to two years old, new foods, tastes and textures should be introduced with the goal of having all children consume foods presented in Eating Well with Canada’s Food Guide by the time they are two years old.
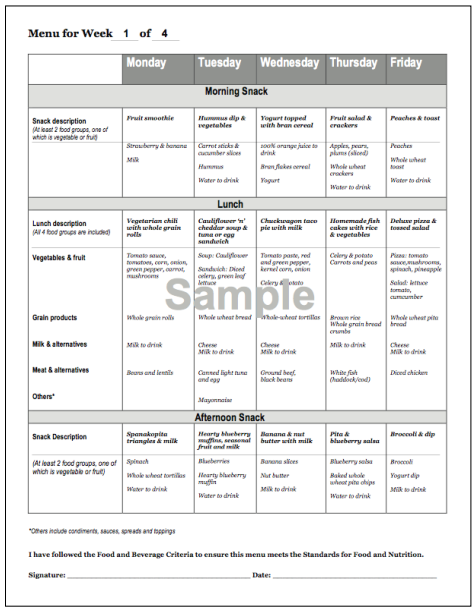
- 1.1 Foods and beverages served are consistent with the Food and Beverage Criteria for Regulated Child Care Settings. The facility director, or the person responsible for menu development, signs and dates the menu to confirm that it complies with the Food and Beverage Criteria.
- 1.2 Full fat milk (3.25% MF) is provided to children under the age of two years.
- 1.3 Menu planning is the responsibility of the facility director or care provider. The facility director may delegate this responsibility to one person, for example, a cook.
- 1.4 Menus are posted in a conspicuous area and identify substitutions that are made.
- 1.5 Menus are developed at least one week in advance of when they will be posted.
- 1.6 All menus and any substitutions made must be kept on file for one year.
Indicators for Licensing
- Menus are posted and signed to confirm that the Food and Beverage Criteria have been followed in the menu development process.
- Substitutions are recorded with a date and kept on file.
2.0 Clean Drinking Water
Water is an essential nutrient. Even mild dehydration can have negative effects on brain function, alertness and energy levels. Eating Well with Canada’s Food Guide encourages drinking water to quench thirst.
- 2.1 Adults and children have access to potable drinking water throughout the day, including when they are engaged in outdoor play and while on off-site outings.
Indicators for Licensing
- Positive Health Inspection Report
- Water is available during outdoor play and on outings.
Resources to Explore
Guidelines for Communicable Disease Prevention and Control for Child Care Settings
Water and Wastewater Facilities and Public Drinking Water Supplies Regulations – Sections 31-35
3.0 Breastfeeding
Nova Scotia along with the World Health Organization, Health Canada and the Canadian Pediatric Society promote breastfeeding as the best way to feed infants for optimal growth and development. It is recommended that infants be exclusively breastfed for the first six months of life, with the introduction of complementary foods at six months and continued breastfeeding up to two years and beyond.
Nova Scotia has a Provincial Breastfeeding Policy that promotes, protects and supports breastfeeding. Providing a supportive environment in regulated child care settings is essential to promote continued breastfeeding.
- 3.1 Regulated child care settings welcome mothers to breastfeed anywhere in the facility or home. A statement to support this is included in the Parent Handbook.
- 3.2 When requested, regulated child care settings provide a comfortable space for breastfeeding mothers (e.g. a chair in a quiet space). A statement to support this is included in the Parent Handbook.
- 3.3 Breast milk is stored in the refrigerator and labeled with the contents, date and the child’s name.
- 3.4 When requested, regulated child care settings work with families to develop an Infant Feeding Plan to address storage and feeding of breast milk. This may also include a plan to follow when the supply runs out and a ‘transition’ plan to other milks if/when necessary. The Infant Feeding Plan is available for review.
Indicators for Licensing
- Parent Handbook includes statement on breastfeeding.
- Bottles are labeled with required information.
- Infant Feeding Plans are on file when applicable.
Resources to Explore
Infant Feeding Plan Appendix C: Resources and Tools
Office of Nutrition Policy and Promotion (ONPP), Health Canada
Provincial Breastfeeding Policy
Make Breastfeeding Your Business: An Action Support Kit
4.0 Adapting the Menu for Infants
When babies are 6 months old they will begin to learn to swallow, chew and pick up solid food. This is a time for getting used to new tastes and textures of food. Infants will explore new foods and learn to enjoy healthy foods. It is important that infants receive nutrient dense, iron containing foods at 6 months of age. This may include foods from the meat and alternative group, including beef, fish, poultry, cooked egg yolks, tofu, and well-cooked legumes.
As infants grow and develop they adjust to the textures of new foods and fewer modifications are required. When infants reach 12 months of age they should be eating most of the same foods as older children. Ongoing communication between the parent/guardian and staff/care provider about the infant’s nutritional needs is important during the transition to new foods.
- 4.1 Upon enrolment, Infant Feeding Plans are created for children between the ages of birth to 17 months, at the request of the parents or when parents provide foods from home.
- 4.2 Infant Feeding Plans, when created, are used for ongoing communication between the infant’s parent/guardian and the care provider or the staff, including the cook.
- 4.3 The Infant Feeding Plan is used to record and communicate the infant’s progress during the transition to solid foods and indicates, when requested by the parent, how menu items are prepared to accommodate the infant’s developmental stage.
- 4.4 Staff and care providers allow infants to explore their food, feed themselves and respond to hunger and fullness cues. A statement to support this is included in the Parent Handbook.
- 4.5 Unless otherwise identified on the Infant Feeding Plan, children who are six months of age or older receive daily meals and snacks that are based on the menu. (Parents may bring food from home during their child’s transition to solid food; however, this is not required and must be identified on an Infant Feeding Plan.)
- 4.6 Iron containing foods as listed in the rationale are included on the menu.
- 4.7 Honey and products containing honey are not served to children who are less than 12 months of age.
Indicators for Licensing
- When applicable, infant feeding plans are available for review.
- Parent Handbook includes a statement on 4.3 with respect to self feeding and following hunger and fullness cues.
- Bottles and foods brought from home are labeled with required information.
Resources to Explore
Infant Feeding Plan Appendix C: Resources and Tools
5.0 Food Safety
Children in group child care settings are at an increased risk for acquiring food borne illnesses. Some of the risk factors associated with food borne illness include poor temperature control, cross contamination and inadequate hygiene. It is essential that regulated child care settings implement sound practices for the prevention of food borne illness. Foods and beverages served in regulated child care settings must comply with applicable food safety regulations to ensure a consistent and safe food environment for children.
- 5.1. Full day child care facilities require a Food Establishment Permit or must purchase food from an establishment that has a Food Establishment Permit.
- 5.2 Regulated child care settings follow the Guidelines for Communicable Disease Prevention and Control for Child Care Settings.
- 5.3 When medical, religious, or cultural beliefs require a child to bring food from home, or when the child is in a school age program where lunch is not provided, foods must be labeled with the child’s name and refrigerated if necessary.
- 5.4 Child care facilities that hold a Food Establishment Permit can only purchase or receive donations of food or beverages in accordance with the Department of Agriculture Food Safety Regulations.
- 5.5 Child care settings that do not hold a Food Establishment Permit can only purchase or receive donations of food or beverages from an establishment permitted by the Department of Agriculture.
- 5.6 Despite Sections 5.4 and 5.5, some foods may be donated to or purchased for regulated child care settings under the following circumstances:
-
- the food is considered to be a low risk food by the Department of Agriculture, including whole fruits and vegetables that have not been cut except for the purpose of harvesting and dry non-potentially hazardous baked goods (i.e. those that do not contain cream, custard, cream cheese, meat or any other potentially hazardous food as a filling or a topping; and
- the food brought into the program is acceptable to the licensee.
- 5.7 Foods that have been donated to or purchased for a facility must:
-
- be labelled with the name of the source of the food;
- include a list of ingredients and any special preparation, storage or serving instructions; and
- (be in accordance with Standard 6 (special dietary considerations).
- 5.8 The Parent Handbook must include a statement on the requirements for foods that have been donated to or purchased for a facility.
Indicators for Licensing
- Food from home is labeled and stored properly.
- Guidelines for Communicable Disease Prevention and Control for Child Care Settings are observed.
- Parent Handbook includes a statement on food purchased for or donated to the facility.
Resources to Explore
Guidelines for Communicable Disease Prevention and Control for Child Care Settings – Section 10 Food
6.0 Special Dietary Considerations
All children need nourishment during the day and should participate in the routine meal and snack times in the child care setting. It is recognized that some children may not be able to eat all of the foods served and may be challenged in following the regular meal and snack routines.
There could be a variety of reasons for this, including life threatening food allergies and other medical conditions that require special dietary considerations to be implemented. It is important that staff and care providers demonstrate openness and a non-judgmental approach toward children’s dietary requirements to ensure that all children receive the nourishment they need in a supportive environment.
- 6.1 Special dietary considerations are identified during the enrolment process and documented on the child’s file.
- 6.2 Food brought from home for a child with special dietary considerations must adhere to any policies and protocols related to special dietary considerations as per 6.3.
- 6.3 Special dietary considerations, including allergy and anaphylaxis information specific to an individual child is communicated to all staff, those who prepare and serve food, care providers, substitutes, volunteers and student interns. This information is posted in the food preparation area and any other places necessary to ensure that those people who need to know this information are able to view it.
- 6.4 Any other protocols, anaphylaxis policies and general information related to special dietary considerations are posted in a clearly visible location in the child care setting
Indicators for Licensing
- If applicable, child’s enrolment information includes information on special dietary considerations.
- Foods and beverages brought from home are identified on the child’s enrolment information.
- Information regarding a child’s special dietary considerations is visibly posted in the appropriate locations.
7.0 Meal and Snack Routines
Healthy meal environments focus on positive meal and snack routines, rather than specific times to eat. While there is a need for routine in respecting children’s appetite, it is important for staff and care providers to be flexible and recognize that children need to eat frequently. An understanding of children’s food intake may be developed by observing and recognizing other factors that may influence their appetite and interest in food (e.g. illness, distractions, foods consumed before arriving at child care).
Maintaining an open line of communication with the child’s parents is essential in understanding issues and challenges that may arise and in ensuring that children’s nutritional needs are met.
- 7.1 Daily meal and snack schedules provide children, staff and care providers with enough time to prepare the eating area, serve the food, consume the food and clean-up.
- 7.2 Staff and care providers are responsive to children’s cues around hunger and provide snacks and meals outside of the regular schedule as required. A statement to support this is included in the Employee Handbook and the Parent Handbook.
Indicators for Licensing
- Daily schedule posted.
- Employee Handbook and the Parent Handbook contain a statement regarding responsiveness to children’s hunger cues.
8.0 Meal and Snack Time Environment
Infants and children are born with the ability to regulate how much food and drink they require for healthy growth and development. Staff and care providers are responsible for what and when children eat, and children are responsible for how much or even if they want to eat. Respecting children’s ability to determine when they are hungry, and when they are full, will promote healthy eating behaviours that will have lasting effects.
It is important that adults sit with the children as they are important role models during meal and snack times. When children are engaged with adults during snack and meal times, and watch adults eating various types of foods, they are more likely to eat the same foods. Over time, when children participate in meal service and serve themselves, they are also more likely to take only the food they require. Meal and snack times provide excellent opportunities to foster children’s self-help and social skill development.
- 8.1 Staff and care providers create a relaxing and enjoyable meal environment (e.g. plan for transitions in routine from play to meal/snack). A statement to support this is included in the Parent Handbook and the Employee Handbook.
- 8.2 For all snacks and meals, child care settings provide safe and sanitary seating and table arrangements with tables, chairs and table settings (e.g. plates, utensils, cups) that are appropriate for the children’s ages and competencies.
- 8.3 Staff and care providers implement appropriate seating accommodations and provide specialized utensils, when needed, for children with special needs.
- 8.4 Children with special needs join their peers for meal and snack times.
- 8.5 Staff and care providers encourage children to respond to hunger and feelings of fullness and children are not forced to finish food that has been served. A statement to support this is included in the Employee or Care Provider Handbook and the Parent Handbook.
Indicators for Licensing
- Employee or Care Provider Handbook and Parent Handbook includes statements on the meal and snack environment and following children’s hunger cues.
- Observed mealtimes are appropriately managed by staff/care provider.
Resources to Explore
Loving Care: 6-12 months and 1 – 3 years – Food Section
9.0 Modelling Positive Attitudes towards Food and Nutrition
The types of foods that children choose and the attitudes that they develop towards food and nutrition, are influenced by their peers and the adults in their lives.
When adults consistently model healthy eating practices and positive attitudes towards food and nutrition, they directly influence and encourage children to develop positive ideas and attitudes about food and nutrition.
Staff and care providers are important role models in regulated child care settings and can influence children’s attitudes toward food and nutrition through their own behaviours and actions with food.
- 9.1 When working directly with children, staff and care providers model healthy eating practices that are consistent with these standards. A statement to support this is included in the Employee Handbook and the Care Provider Handbook.
Indicators for Licensing
- Observed mealtimes are appropriately managed by staff/care provider.
- Employee Handbook or Care Provider Handbook includes a statement regarding the expectations for staff/care providers during meal and snack times.
Resources to Explore
Loving Care: Parents and Families – Section on Eating for Wellness
10.0 Fundraising with Food and Beverages
Regulated child care settings often fundraise to purchase materials and equipment that will enhance the programs they offer. Fundraising with healthy food and beverages, or non-food items, provides an opportunity for licensees, staff and care providers to promote positive nutrition messages that reflect these standards.
This will help to ensure that the messages that children receive around health and nutrition in child care are consistent with the messages they hear at home and in the broader community.
- 10.1 When fundraising occurs in facilities during operating hours, the items are non-food items, or food and beverages that comply with the Food and Beverage Criteria.
Indicators for Licensing
Fundraising during operating hours complies with expectations set out in the Food and Beverage Criteria.
Resources to Explore
Manual for Food and Nutrition in Regulated Child Care Settings
11.0 Food is Not Used to Reinforce Desired Behaviours
Children are served best when they are supported to develop competence, self awareness, and a sense of self-worth in their child care setting. Ensuring that there are many opportunities for children to develop trusting and genuine relationships with the adults and peers in their child care setting will contribute to this. Children display positive behaviours and meaningful activities when the environment reflects their interests, is child-centered and play-based.
When children are respected for who they are and are supported by caring adults and peers to resolve difficult situations, external motivators, such as food, are not required. Using food as a motivator teaches children that food is associated with an action and not with hunger. It can teach children to prefer some foods over others and can alter children’s natural ability to respond to internal cues that allow them to know when they are hungry and when they are full.
- 11.1 The licensee’s Behaviour Guidance Policy states that:
(i) Staff, volunteers and care providers do not offer food to reinforce positive behaviours.
(ii) Staff, volunteers and care providers do not withhold food as a consequence for inappropriate behaviours.
(iii) Food is not used as a reward for completing a task or finishing a meal (e.g. dessert will not be withheld if the child does not finish the main meal).
- 11.2 When a child’s team (which may include staff, external professionals and the child’s parents/guardians) has determined that food is the most appropriate and natural way to reinforce desired behaviours and support the child’s development, then a routine-based plan (RBP) must be developed for the child. The RBP must include a plan for replacing and/or reducing the use of food as a motivator.
Indicators for Licensing
- Behaviour Guidance Policy includes the required statements.
- Routine Based Program Plans include the above if appropriate.
12.0 Special Functions
Special occasions and celebrations create opportunities for children and adults in a child care setting to build relationships and get to know each other. Food is often a symbol of community and kinship during special occasions and celebrations.
- 12.1 Any policies and protocols related to special dietary considerations, in accordance with Section 6, are followed.
- 12.2 Foods and beverages served at special functions during regular operating hours (e.g. Valentine’s Day, Halloween, and birthday celebrations) are identified on the menu in advance of the celebration and comply with the Food and Beverage Criteria.
Indicators for Licensing
- Menus are posted and appropriately signed indicating the Food and Beverage Nutrient Criteria have been met.
13.0 Promotion and Advertising
Marketing to children has a strong influence on the food that children choose. The Internet, television, games, toys, and character placement on food products, clothing, utensils and placemats make it easy for food companies to market their products to children. This allows companies to create brand loyalty that will last into adulthood. Food and beverages that are marketed to children are often of poor nutritional quality and negatively impact on children’s food preferences.
Regulated child care settings have a responsibility to nurture healthy childhood growth and development, which includes creating an early learning environment that fosters healthy food preferences.
- 13.1 Promotional materials that are intended to advertise specific brands or characters are not used to serve meals and snacks.
Indicators for Licensing
- Promotional materials are not used to serve meals and snacks.
Section B: Guidelines for Food and Nutrition in Regulated Child Care Settings Government of Nova Scotia
Guidelines are based on evidence and best practices. Guidelines are not mandatory but provide suggestions for recommended courses of action in regulated child care settings.
1.0 Family Involvement and Communication
It is important for families and regulated child care settings to work together to ensure that young children eat well and develop positive attitudes towards healthy foods and nutrition. For these Standards for Food and Nutrition in Regulated Child Care Settings to be successful, it is important that families and child care work together to understand and implement them.
- 1.1 Regulated child care settings welcome families to participate in snacks and meals when possible.
- 1.2 Regulated child care settings provide families with recipes when requested.
- 1.3 Regulated child care settings invite families to participate in educational opportunities to learn about the Standards for Food and Nutrition in Regulated Child Care Settings and the importance of healthy attitudes towards eating and nutrition in early childhood (e.g. parent-teacher nights).
- 1.4 Staff and care providers create opportunities for families to share ideas and information on inclusive healthy food and nutrition practices, religious practices and cultural beliefs.
- 1.5 Regulated child care settings recognize the strengths and resources that families can offer in enabling the setting to comply with the Standards for Food and Nutrition.
2.0 Creating Opportunities for Children to Learn About Nutrition
Children learn about food and nutrition through natural play experiences that emerge during the daily routine. Through observation and by listening to children, staff and care providers can build upon children’s knowledge of and interest in healthy foods and nutrition. Through play and meaningful activities, children can explore and investigate their ideas about health and nutrition, building upon their interest in and understanding of the importance of healthy eating and the wide variety of foods that may be found locally and around the world.
- 2.1 When opportunities occur naturally (“teachable moments”) to share food and nutrition information with children, staff and care providers foster children’s understanding of healthy eating and food choices.
- 2.2 Staff and care providers build upon and expand children’s natural interest in food and nutrition concepts beyond meal and snack times (e.g. preparing food with the children, planting a garden, composting, exploring new foods).
- 2.3 Children learn about breastfeeding as the natural and healthiest way to feed a baby.
- 2.4 Staff and care providers create an environment that encourages learning, understanding and respect for diversity. Children have opportunities to learn about food and eating practices in many cultures.
- 2.5 Staff and care providers model and promote respectful practices toward food to ensure minimal food waste. Non-food items are used for art activities, sensory play and games.
3.0 Nova Scotia Produce and Products
Nova Scotia produces an abundance of produce and food products. Buying food that is grown and produced within the province supports Nova Scotia agriculture and business and means that more money remains in the community. Locally grown, fresh food is often more nutritious if it is used shortly after harvest.
- 3.1 When possible, regulated child care settings serve local, seasonal food and beverages that are harvested, produced, or manufactured in Nova Scotia and Atlantic Canada.
4.0 Food Packaging and Environmental
As future leaders and stewards of the earth, it is important for young children to learn about the importance of leading an environmentally friendly lifestyle. This encompasses an understanding of the value in composting and reducing waste. Nova Scotia is noted for its commitment to composting and recycling. Many communities and families teach their children the value of reducing, reusing and recycling. It is important to ensure that children receive consistent messages with respect to the environment in both home and child care settings.
- 4.1 Licensees encourage staff and care providers to find ways to reduce consumer and food waste.
- 4.2 Licensees encourage and support staff and care providers to use energy-saving practices (e.g. energy saving equipment such as fridges and stoves that meet the Energy Star standard).
- 4.3 When possible, licensees ensure that staff and care providers use food-safe bulk containers rather than individual containers (e.g. pitchers/cartons of milk will be used rather than individual containers).
- 4.4 When possible, licensees ensure that staff and care providers use reusable dishes and cutlery. When this is not possible, child care facilities and family day care homes ensure that dishes can be recycled or composted.
- 4.5 Licensees strive to minimize food waste in regulated child care settings through appropriate menu planning and food preparation.
5.0 Food for Staff and Care Providers
Staff and care providers may bring food for their own consumption into the child care setting. It is important to recognize that children view adults as role models and often want to copy adult behaviour. Children will want to eat the same kinds of foods as they see the adults in their lives eating.
- 5.1 Regulated child care settings develop a clear policy for staff and care providers regarding foods brought into the setting. The policy must be consistent with all food related policies and protocols that are in place.
- 5.2 When eating with children, staff and care providers choose the same foods as the children unless they have special dietary considerations that prevent them from doing so.
Section C: Food and Beverage Criteria in Regulated Child Care Settings
In accordance with Section 1 of the Standards for Food and Nutrition, the Food and Beverage Criteria must be followed when creating a menu. The criteria will guide you in creating a menu that will meet requirements set out in both the Day Care Regulations and the Standards. One of these requirements is to ensure the foods served in regulated child care settings follow Eating Well with Canada’s Food Guide. The pattern of healthy eating outlined in the Food Guide will contribute to the optimal growth and development of the children.
The Food and Beverage Criteria were developed based on international and national recommendations and guidelines from the Institute of Medicine (Dietary Reference Intakes), Health Canada, Canadian Pediatric Society, Heart and Stroke Foundation and Dietitians of Canada, in addition to similar policies and guidelines in other provinces, territories and jurisdictions.
Total fat, saturated and trans fat, sodium and sugar are the focus of these criteria as they influence health outcomes such as obesity, diet-related cancers, diabetes, high blood pressure and dental problems. Foods that are high in total fat, saturated and trans fat, sodium and sugar can take the place of healthier foods and as a result won’t give toddlers and preschoolers the nourishment they need to grow and develop.
Research has shown that when children are exposed to and consume fatty, salty and sweet foods, they may prefer them over healthier foods. For these reasons, the Food and Beverage Criteria will guide the selection and preparation of foods that are low in total fat, saturated fat, sodium and sugar. A more thorough explanation regarding the specific nutrients of concern is provided in Appendix A.
How to use the Food and Beverage Criteria
These food and beverage criteria are based on Eating Well with Canada’s Food Guide. The Food and Beverage Criteria include the Foods to Serve, Nutrient Criteria tables, Food Preparation Tips and Foods Not to Serve.
- Review the current menu to ensure that the foods served meet the Food and Beverage Criteria. Or, photocopy and use the Menu Template in the Resources and Tools section to create a new menu. A new menu can be created each week or a series of menus can be created and rotated. Offer a variety of foods from the four food groups on all days of the week. Once the menu is completed, sign and date it to confirm that it meets the Food and Beverage Criteria. See example on page C5.
- Use the Foods to Serve lists to help choose foods for the menu as well as for ideas on how to prepare these foods in a healthy way. If a food is on the Foods to Serve list, it can be included on the menu and it is not necessary to look at the Nutrient Criteria for these foods.
- Use the Nutrient Criteria to determine if foods that are not on the Foods to Serve
list can be included on the menu. - Use the Nutrient Criteria to identify which packaged foods can be included on the menu. While packaged foods are convenient, they are often high in fat, salt and/or sugar or contain sugar substitutes, and are low in nutritional value. If the packaged food does not fit the criteria, it should not be included on the menu.
Menu Checklist
The Menu Checklist can be used as a starting point to create a menu, and as a final check once the menu is completed to ensure all the criteria have been met.
Recipes
- Individual ingredients in the recipe fit within the Foods to Serve lists or the Nutrient Criteria tables.
- Items on the Foods Not to Serve lists are not included in recipes.
- Use the list of Healthy Substitutions (Appendix B) to reduce or eliminate fat, salt and sugar in recipes.
Balance and Variety
- At least one serving* from each of the four food groups is served at meal time.
- At least two of the four food groups are included at every snack.
- Meal and snack items within the same day and from day to day include variety in terms of:
- colour (e.g. neutrals, oranges, greens, reds) flavour (e.g. strong or mild; sweet or sour)
- texture (e.g. crisp or soft)
- shape (e.g. natural, round, cubes, sticks)
- temperature (e.g. cold or hot)
*Refer to Appendix A for more information on Food Guide Servings and portion sizes.
Vegetables and Fruit
- All snacks include at least one serving from the Vegetables and Fruit Food Group
- In full day child care settings, at least one dark green vegetable or one orange vegetable or fruit is served each day (see Foods to Serve lists for examples).
- 100% juice is served no more than two times a week (½ cup per serving).
- A variety of vegetables and fruit are served each day.
Grain Products
- In full day child care settings, a minimum of half the grain products served each day are whole grain.
Milk and Alternatives
- Children under two years of age are served whole/homogenized (3.25%) milk.
- In full day child care settings, one cup of fluid milk should be offered to each child every day. This could be divided into two 1/2 cup (125 mL or 4 oz) servings a day for children to ensure they will eat the foods at the meals and snacks as well.
Meat and Alternatives
In full day child care settings:
- Meat alternatives are served at least once a week (e.g. dried beans, lentils, tofu).
- Fish is served at least once a week.
- A variety of meats and alternatives are served throughout the week (e.g. poultry, eggs, beef, pork, fish, beans, peas, lentils, tofu).
Other
- Plain water is available throughout the day as well as during snacks and lunch.
- Condiments (e.g. salsa, cream cheese, parmesan cheese, sour cream, jam, ketchup, chutney, croutons, unsweetened cocoa powder, feta, brie, and blue cheese) are used sparingly as minor ingredients (e.g. 1 teaspoon (5 mL) to 1 tablespoon (15 mL) per serving).
- Packaged foods on your menu fit within the Foods to Serve lists or Nutrient Criteria.
- Foods from the Foods Not to Serve lists are not included on the menu.
- The quantity of foods from each food group included in a mixed dish is sufficient to count as a serving* for every child. (If you serve chicken noodle casserole for lunch, there needs to be enough chicken to count as a serving from the Meat and Alternatives food group for each child).
Vegetables and Fruit
- All snacks include at least one serving from the Vegetables and Fruit Food Group.
- In full day child care settings, at least one dark green vegetable or one orange vegetable or fruit is served each day (see Foods to Serve lists for examples).
- 100% juice is served no more than two times a week (½ cup per serving).
- A variety of vegetables and fruit are served each day.
If a product is packaged, it must fit within the Foods to Serve list or the Nutrient Criteria.
Foods to Serve
- Fresh vegetables
- Frozen vegetables (no added sodium or fat)
- Canned tomatoes, whole, diced or crushed (look for no added sodium or low sodium)
- Canned vegetables (rinsed and drained)
- Fresh fruit
- Frozen fruit (100% fruit, no added sugar)
- Canned fruit (packed in juice or light syrup)
- Dark green vegetables include:
- asparagus, green beans, bok choy/Chinese cabbage, broccoli, Brussels sprouts, edamame, fiddle heads, endive, kale/collards, leeks, lettuce (romaine), mesclun mix, mustard greens, okra, peas, green pepper, seaweed, snow peas, spinach, zucchini
- Orange vegetables and fruit include:
- carrots, pumpkin, squash, sweet potato, yam, apricot, cantaloupe, mango, nectarine, papaya, peach
- Apple sauce and other fruit sauces (100% fruit, no added sugar or sugar substitutes)
- Dried fruit and vegetables without added sugars, sugar substitutes or fat
Packaged foods can be high in sodium, fat and/or sugar. Some packaged foods can be served if they fit within the criteria below.
| Nutrient Criteria: Vegetables and Fruit (per Food Guide Serving) |
|||||
| Food | Serving size | Sodium | Fat | Sugar | Examples |
| Prepared vegetables, frozen |
½ cup 110 g or 125 mL | ≤ 360 mg | ≤ 3 g total fat, 2 g or less of saturated and trans fat combined | no added sugar | Frozen vegetables such as french fries, vegetables with sauce |
| 100% vegetable and fruit juices/blends or 100% frozen unsweetened juice bars |
½ cup | ≤ 240 mg | N/A | no added sugar | Vegetable juices such as carrot, tomato, vegetable blends |
| Fruit juices such as orange, pineapple, apple, etc | |||||
| Frozen bars made with 100% real juice | |||||
Note: ≤ this symbol means less than or equal to.
Food Preparation Tips
- Prepare vegetables and fruit with little or no added fat, sugar or salt.
- Enjoy vegetables steamed, roasted or stir-fried.
- Leave the skin on new carrots and potatoes as a way to keep the fibre.
- Add vegetables like cucumber, peppers, mushrooms, and celery to sandwich fillings.
- Use orange vegetables such as carrots, squash or yams to make soup.
- Add vegetables to your pizza, like peppers, mushrooms, pineapple, onions, broccoli and tomatoes.
- Drain and rinse canned vegetables in cold water for 30 seconds to reduce the sodium content.
- Choose spices, herbs and reduced sodium broth, instead of regular broth and salt when making soups.
- Choose reduced sodium sauces (e.g. soy sauce, hoisin sauce).
- Use spices and herbs to season vegetables instead of fat or salt.
- Rinse and drain fruit canned in syrup to reduce sugar content.
- Chop or dice dried fruits into small pieces to reduce choking risk.
Foods Not to Serve
These foods should not be included on the menu:
- Fruit-based drinks that contain less than 100% fruit juice. (e.g. fruit drinks, fruit punch, fruit beverages, fruit-flavoured drinks, lemonade)
- Battered vegetables (e.g. battered zucchini)
- Sweetened gelatin/jellied desserts
- Pickles
- Dried vegetables or fruit with added sugar and/or sugar substitutes
Grain Products
- In full day child care settings, a minimum of half the grain products served each day are whole grain. Grain products are considered whole grain if:
- the ingredient list of prepackaged grains includes whole grains as the first ingredients listed OR
- your recipe includes whole grains (e.g. whole grain flour, oats, cornmeal, cracked wheat, quinoa)
If a product is packaged, it must fit within the Foods to Serve list or Nutrient Criteria.
Foods to Serve
Oats, corn, rice, wheat berries, flax seeds, wheat germ, rye, light rye, stone ground whole wheat, kamut, amaranth, quinoa, pumpernickel, barley, cracked wheat, bulgur, sprouted grain, flax, wheat germ
- Whole grains
- Rice (no added salt)
- Couscous
Packaged foods can be high in sodium, fat and/or sugar. Some packaged foods can be served if they fit within the criteria below.
| Nutrient Criteria: Grain Products (per Food Guide Serving) | ||||||
| Food | Serving size | Sodium | Fat | Sugar | Fibre | Examples |
| Bread products | 1 slice bread (35 g), ½ bagel (45 g), ½ pita or tortilla (45 g) | ≤ 240 mg | ≤ 2 g saturated & trans fats combined | ≤ 8 g | ≥ 1.6 g | Breads, buns, rolls, bagels, tortillas, chapatti, roti, naan, bannock, pita, buns, english muffins, tortillas |
| Ready-to-eat cold and hot cereals | cold cereal, ¾ cup – 1 cup (175-250 mL) or prepared hot cereal ¾ cup (175 mL) | ≤ 350 mg | ≤ 2 g saturated & trans fats combined | ≤ 11 g | ≥ 2 g | Wheat squares, oat, O’s, oatmeal |
| Crackers | 30 g | ≤ 360 mg | ≤ 2 g saturated & trans fats combined |
≤ 2 g | ≥ 1.6 g | Whole wheat or whole grain crackers |
| Rice crackers, rice cakes | 30 g | ≤ 280 mg | ≤ 2 g saturated & trans fats combined |
N/A | N/A | Plain rice cakes, plain rice crackers |
| Pasta (fresh or dried, no condiments or filling) |
85 g dry serving* | ≤ 140 mg | ≤ 2 g saturated & trans fats combined | N/A | ≥ 3 g | Whole wheat pasta including macaroni, spaghetti, lasagna, penne, pasta side dish |
| Baked goods (fresh or frozen, no sweetened fillings) | 35 g | ≤ 250 mg | ≤ 2 g saturated & trans fats combined | ≤ 50% carbohydrate from sugar | ≥ 2 g | Fruit or vegetable based muffins, scones or loaves, granola bars |
| Pancakes and Waffles | 35 g | ≤ 115 mg | ≤ 2 g saturated & trans fats combined |
≤ 5 g | ≥ 1 g | Frozen pancakes or waffles |
Note: ≤ this symbol means less than or equal to; ≥ this symbol means greater than or equal to.
*This is a packaged serving size, not a Food Guide serving
Food Preparation Tips
- Add brown or wild rice to soups, salads and casseroles.
- Prepare baked goods with whole grains (e.g. whole wheat flour, rolled oats).
- When baking, use vegetable oils such as canola, olive and soybean.
- Choose soft margarines that are low in saturated and trans fats (e.g. non-hydrogenated margarine).
- Prepare muffins with bran and fruits.
- Use whole wheat pasta in macaroni and cheese and other casseroles.
- Use whole wheat pizza crusts and tortilla wraps.
- Prepare grain products with little or no added fat, sugar and salt (See Healthy Substitutions, Appendix B).
Foods Not to Serve
These foods should not be included on the menu:
- Baked goods and other grain products with sugar substitutes
- Foods containing honey to those 12 months and younger
- Hard taco shells
- Pastries and doughnuts
Milk and Alternatives
- Children under 2 years of age are served whole/homogenized (3.25%) milk.
In full day child care settings, one cup of fluid milk should be offered to each child every day. - This could be divided into two 1/2 cup (125 mL or 4 oz) servings a day for children to ensure they will eat the foods at the meals and snacks as well.
Foods to Serve
- Milk (including fluid, powdered and canned evaporated milk)
- Plain fortified soy beverage (children 2 years of age and older)
- Ricotta cheese (plain)
- Cottage cheese (plain)
Packaged foods can be high in sodium, fat and/or sugar. Some packaged foods can be served if they fit within the criteria below.
| Nutrient Criteria: Milk and Alternatives (per Food Guide Serving) |
||||
| Food | Serving Size | Sodium | Sugar | Examples |
| Yogurt or kefir | ¾ cup/175 g | ≤ 140 mg | ≤ 30 g | Plain or fruit flavored yogurt |
| Yogurt beverage | 200 mL | ≤ 140 mg | ≤ 30 g | Flavored yogurt beverage |
| Cheese* | 1 ½ oz (50 g) | ≤ 480 mg | N/A | Cheddar, mozzarella, Swiss, brick |
| Ricotta cheese | 55 g* | ≤ 240 mg | No added sugar | Plain ricotta cheese |
| Puddings and custards | ½ cup (125 mL) | ≤ 450 mg | ≤ 30 g | Ready-to-eat or prepared from mix |
| Flavoured milk or soy beverage | 1 cup/250 mL | ≤ 200 mg | ≤ 28 g | Chocolate milk, vanilla or chocolate soy beverage |
Note: ≤ this symbol means less than or equal to.
*This is a package serving size and not a Food Guide Serving.
Food Preparation Tips
- Add milk and/or yogurt to smoothies.
- Use yogurt as a base when making dips.
- Use milk or yogurt in baked goods.
- Serve milk-based soups and chowders.
- Use yogurt as a dip for fruit.
- Shred cheese such as mozzarella and include in sandwiches, salads and wraps, and on baked potatoes.
- Choose reduced sodium cottage cheese and ricotta.
- Freeze yogurt smoothies for a cool snack.
Foods not to Serve
These foods should not be included on the menu:
- Low fat or non-fat milk to children younger than 2 years of age.
- Yogurt containing sugar substitutes.
- Ice cream and frozen desserts.
- Processed cheese spreads and slices.
Meats and Alternatives
In full day child care settings:
- Meat alternatives are served at least once a week (e.g. beans, lentils, tofu).
- Fish is served at least once a week.
- A variety of meats and alternatives are served throughout the week (e.g. poultry, eggs, beef, pork, fish, beans, peas, lentils, tofu).
Foods to Serve
- All dried, frozen and canned (rinsed and drained) legumes (e.g. beans, peas, lentils, chickpeas)
- Fresh fish
- (e.g. capelin, char, haddock, hake, herring, Atlantic mackerel, mullet, salmon, smelt, rainbow trout, lake whitefish, blue crab, shrimp, clam, mussels, tongol)
- Canned fish (e.g. canned light tuna made from skipjack or yellowfin)
- Nut and seed butters (e.g. peanut butter, almond butter)
- Nuts and seeds (not served to children under 4 years old)
- Eggs
- Fresh lean meats (e.g. beef, venison, bison, pork, lamb)
- Fresh poultry (e.g. chicken, turkey, duck) (skin removed)
- Hummus and bean dips
Packaged foods can be high in sodium, fat and/or sugar. Some packaged foods can be served if they fit within the criteria below.
| Nutrient Criteria: Meats and Alternatives (per Food Guide Serving) | ||||
| Food | Serving Size | Sodium | Fat | Examples |
| Poultry (frozen, plain, seasoned, coated) |
2 ½ oz (75 g or 125 mL) |
≤ 216 mg | ≤ 12.75 g total fat | Fresh, frozen, plain, unseasoned poultry, with or without skin |
| Fish, seafood or shellfish (frozen, plain, seasoned, coated) |
2 ½ oz (75 g or 125 mL) |
≤ 216 mg | ≤ 3.5 g saturated and trans fat combined | Fresh or frozen haddock, salmon, herring, halibut, trout, shrimp, mackerel, canned light tuna |
| Beef, pork, lamb (frozen, seasoned, etc) | 2 ½ oz (75 g or 125 mL) |
≤ 216 mg | ≤ 12.75 g total fat, ≤ 4.5 g saturated fat |
Fresh or frozen meat |
| Processed meats | 2 ½ oz (75 g or 125 mL) |
≤ 490 mg | ≤ 7.5 g total fat, saturated and trans fat 5% or less of total fat |
Luncheon meats, sliced turkey, chicken, ham, roast beef, canned meat |
| Liquid eggs | ¼ cup (61 g) | ≤ 115 mg | ≤ 3.7 g | Liquid egg |
| Legumes (prepared) | ¾ cup (175 mL) | ≤ 500 mg | N/A | Baked beans, bean salads |
| Vegetarian, products (soy, tofu, etc) | 2 ½ oz (75 g or 125 mL) |
≤ 450 mg | ≤ 7.5 g total fat, ≤ 2 g saturated and trans fat combined |
Veggie ground beef, veggie burgers, tofu |
Note: ≤ this symbol means less than or equal to.
Food Preparation Tips
- Bake, broil, boil, poach or roast meat, poultry, and fish.
- Drain excess fat from cooked meat or poultry.
- Drain and rinse canned legumes in cold water for 30 seconds to reduce the sodium content.
- Prepare lean meat and alternatives with little or no added fat or salt.
- When buying whole chicken or chicken pieces, remove the skin before cooking.
- Use whole wheat bread crumbs or crushed whole grain cereal when making bread coatings.
- Serve hummus and pita wedges as a snack.
- Offer hard-boiled eggs or egg salad as a snack.
- Include tofu and/or legumes (e.g. chick peas) in stir fries.
- Serve lentil or split pea soups.
- Add dried beans and peas to soups, stews, and salads and chili.
Foods not to Serve
These foods should not be included on the menu:
- Hot dogs, bologna, salami, pepperoni, bacon and sausages
- Nuts and seeds to children under the age of four years*.
- Fish with bones*
- High mercury fish:
- Limit fresh/frozen tuna, shark, swordfish, marlin, orange roughy and escolar to 75 g or one Food Guide serving a month.
- Limit canned albacore (white) tuna** to 75 grams or one Food Guide serving a week.
* Choking hazard
**Does not apply to canned light tuna.
Mixed Dishes and Other Foods
Mixed dishes (e.g. casseroles, stews, lasagna) have ingredients from at least two of the four food groups. When a mixed dish is packaged, it must fit within the Foods to Serve list or Nutrient Criteria.
If lasagna is served, it needs to fit within the Nutrient Criteria and also include enough vegetable and/or meat to count as a serving for each child. It may also be used as a serving of grain if there is a sufficient quantity of pasta for each child.
If chicken noodle casserole is served for lunch, there needs to be enough chicken to count as a serving from the Meat and Alternatives food group for each child. A vegetarian pizza would have to have enough vegetables to count as at least one vegetable serving.
Foods to Serve
- Homemade pizza, casseroles, lasagna, chowders and soups, etc.
Packaged foods can be high in sodium, fat and/or sugar. Some packaged foods can be served if they fit within the criteria below.
| Nutrient Criteria: Pre-packaged Mixed Dishes (per Food Guide Serving) | ||||
| Food | Serving Size | Sodium | Fat | Examples |
| Dinners/mixed entrées | 1 cup (250 mL) | ≤ 720 mg | ≤ 2 g saturated fat trans fat, ≤ 5% of total fat |
Prepared stews, chili, dahls, casseroles, lasagna, Shepherd’s pie, etc |
| Pizza | 1 slice (140 g) | ≤ 480 mg | ≤ 10 g trans fat, ≤ 5% of total fat |
Prepared pizza (frozen or fresh) |
| Soups and chowders | 1 cup (250 mL) | ≤480 mg | ≤2 g saturated fat, Trans fat ≤5% of total fat |
Corn or seafood chowder, broth or cream based soups |
| Sauces | ¾ cup (175 mL) | ≤ 750 mg | ≤ 3 g saturated fat, trans fat ≤ 5% of total fat | Meat, vegetarian, tomato or cream sauces |
Note: ≤ this symbol means less than or equal to.
Other
Oils and fats
- Use vegetable oils such as canola, olive and soybean. This includes oils and fats used for cooking, salad dressings, and for spreads.
- Choose soft margarines that are low in saturated fat and trans fat. Avoid butter, hard margarine, lard, shortening and gravy.
Condiments
- Condiments (e.g. salsa, cream cheese, parmesan cheese, bread crumbs, sour cream, jam, ketchup, chutney, croutons, unsweetened cocoa powder, feta, brie, and blue cheese) are used in small amounts to enhance flavours and do not fit within the Food Guide as a Food Guide Serving. As such, small amounts are defined as 1 tsp (5 mL) to 1 tbsp (15 mL).
Recipes
- When cooking or baking, there are a few things to look for in order to decide if a recipe fits the criteria. If the following are met, then your recipe fits and can be included on the menu:
- Individual ingredients* in the recipe fit within the Foods to Serve lists or the Nutrient Criteria.
- Items on the Foods Not to Serve lists are not included in recipes.
- Use the list of Healthy Substitutions (Appendix B) to reduce or eliminate fat, salt and sugar in recipes.
*Flours, sugar, buttermilk, spices, leavening agents (baking soda and baking powder), etc are not listed on the Foods to Serve lists as they are not typically consumed on their own, but are allowed in recipes as ingredients.
Foods Not to Serve
The following foods will not be included on the regular daily menu as ingredients or as foods served. These foods are typically high in fat, sodium and/or sugar, may contain sugar substitutes and are low in nutritional value.
- Fruit-based drinks that contain less than 100% fruit juice. (e.g. fruit drinks, fruit punch, fruit beverages, fruit-flavoured drinks, lemonade)
- Battered and fried vegetables (e.g. battered zucchini)
- Sweetened gelatin (jellied desserts)
- Pickles
- Dried vegetables or fruit with added sugar and/or sugar substitutes
- Hard taco shells
- Pastries and doughnuts
- Ice cream and frozen desserts (e.g. freezies and popsicles)
- Processed cheese spreads and slices
- Low fat or nonfat milk to children younger than 2 years of age
- Hot dogs, bologna, salami, pepperoni, bacon and sausages
- Foods or beverages containing sugar substitutes (e.g. yogurt, baked goods)
- Candy and chocolate, including chocolate spreads
- Marshmallows
- Snack foods (e.g. potato chips, tortilla chips, cheese puffs, pretzels)
- Pop, diet pop
- Sport and energy drinks
- Water with added flavourings, sweeteners, vitamins, minerals, etc.
- Beverages with caffeine or alcohol should never be served to children
Food Safety
The following foods pose a risk and will not be included on the menu:
- Honey is not safe for infants under 12 months, due to the risk of infant botulism. Do not give infants honey, or any kind of food made with honey, for the first year. This includes baked and cooked items that contain honey.
- Unpasteurized food and beverages
- Homemade canned goods
- High mercury fish:
- Limit fresh/frozen tuna, shark, swordfish, marlin, orange roughy and escolar to 75 g or one Food Guide serving a month.
- Limit canned albacore (white) tuna* to 75 grams or one Food Guide serving a week.
*Does not apply to canned light tuna.
Choking Hazards
The following foods are potential choking hazards for children younger than 4 years of age:
- Nuts, popcorn
- Hard candy, cough drops, gum
- Whole grapes, raisins
- Carrots cut into rounds
- Hot dog
- Fish with bones
- Snacks with toothpicks or skewers
- Marshmallows
Some of these foods can be served in a way that makes them safer for young children to eat, for example:
| Foods that can cause choking | Suggestions to make these foods safer |
| Sticky spreads like peanut butter, tahini and almond butter | Spread them thinly on bread or crackers, do not give spoonful of these foods |
| Hard foods like some raw vegetables and fruit | Cook hard foods to soften them, grate them into small pieces |
| Round, smooth foods like grapes and cherries | Cut each one into four small sections, remove seeds or pits |
| Tube-shaped foods like cooked baby carrots | Cut them lengthwise into strips, cut the strips into small pieces |
| Stringy or chewy foods like meat, long thin pasta and melted cheese | Cut these foods into small pieces |
| Dried fruit | Chop or dice into small pieces |
Background for Food and Beverage Criteria
Fat
Fat is an important part of a healthy diet because it provides essential fatty acids and energy (calories). It also helps the body absorb fat soluble vitamins including A, D and E. Eating Well with Canada’s Food Guide recommends that nutritious foods not be restricted because of their fat content for young children. They are growing and have relatively high energy needs and may require healthy higher fat choices from the four food groups.
High fat foods can help children meet their energy needs for growth and development, especially children who eat a small quantity of food. Research also suggests that, for this age group, a low fat diet could lead to inadequate intake of certain nutrients (e.g. vitamins). For this age group, the type of fat is more important, than the amount, in determining health outcomes.
Healthy fats include polyunsaturated and monounsaturated fats. These fats are found in vegetable oils, nuts and seeds, fish, flax and non-hydrogenated margarines. These fats help to lower the risk of heart disease in children and adults. For this reason, healthy fats are included in Canada’s Food Guide as part of a healthy diet.
Saturated and trans fats are unhealthy fats and can increase the risk of heart disease in children and adults. Saturated and trans fats should be avoided or reduced. Saturated fats also raise blood levels of “bad” cholesterol. Saturated fats are found in high fat milk and milk products (e.g. butter and cream), fatty meats (e.g. hot dogs, bologna, salami, pepperoni, ribs, regular ground beef) and tropical oils (palm kernel, coconut oil in store- bought cookies, crackers, granola bars).
Naturally occurring trans fats are found in very small amounts in dairy products as well as beef and lamb.
Artificial trans fats are made when liquid oil is changed into a solid fat (e.g. hydrogenated fats). These hydrogenated fats are found in many processed baked goods (e.g. store bought muffins, cookies, cakes, pastries), deep fried and battered products (e.g. french fries, chicken nuggets, fish sticks), some crackers, shortening products, and hard margarines.
To reduce the amount of trans fats, choose products made without hydrogenated or partially hydrogenated oils.
After two years of age, children can start to transition towards lower fat milk and milk products as their growth slows.
The Food and Beverage Criteria will guide you to choose healthy fats as well as avoid unhealthy fats in your menu.
Fibre
The Adequate Intake (AI) for fibre is 19 grams/day for children between the ages of 1 and 3 and 25 grams/day for children between the ages of 4 and 8.3 Canadian children do not eat enough fibre.2 Ensuring that children eat enough fibre can help to prevent obesity, diabetes, diet-related cancers and reduce the risk of heart disease and constipation. Whole grains, vegetables and fruit, and legumes are high in dietary fibre. Fruit juice is lower in fibre compared to whole vegetables and fruit, and therefore whole vegetables and fruit should be eaten more often than juice.
Eating Well with Canada’s Food Guide recommends that at least half of the grains consumed each day be whole grains. Whole grains provide fibre and other nutrients that children need for healthy growth and development. Having a wide variety of whole grains on the menu will help ensure children are meeting their nutritional needs. The Food and Beverage Criteria will help in selecting whole grains as well as other grain products that are nutritionally dense and rich in fibre.
Sodium
Children 4-8 years old should consume no more than 1900 mg sodium per day. Toddlers and infants should consume even less (1500 mg/day). Eating too much sodium can lead to high blood pressure and other health problems. The Canadian Community Health Survey (2004) revealed that the sodium intake of children one to eight years of age exceeds the recommended limits, which increases their risk of adverse health effects.
Most of the sodium we eat comes from processed, packaged foods, so the Food and Beverage Criteria will provide guidance to help you select low sodium foods and recipes for your menu.
Sugar
Some very nutritious foods naturally contain sugar, such as fruit and milk. Sugars are also added to many products to increase their sweetness. Added sugars are found in sweetened beverages such as fruit punch, sodas and some milk based beverages. Candies, chocolate, sweet desserts and syrups, are other sources of added sugars. Added sugars are indicated in the Ingredient List of product labels. Examples include cane juice, syrup, dextrose, fructose, sucrose, glucose, maltose, lactose, fruit juice concentrate.
International and national recommendations recommend choosing foods and beverages without added sugars to maintain a healthy weight, decrease cardiovascular risk, avoid dental problems and meet nutritional needs. Total sugar intake can be limited by reducing intake of foods and beverages containing naturally occurring sugars (milk, milk products and fruits) and limiting foods and beverages with added sugars.
Although a healthy choice, vegetable and fruit juices contain naturally occurring sugar. Research has shown that drinking too much juice may lead to early childhood tooth decay, diarrhea and being overweight. Drinking too much juice can also replace other nutrient dense foods. Children may fill up on juice and not eat their snacks or meals. For these reasons, it is recommended that children drink water or plain milk in place of juice and to limit juice to no more than ½ cup (125 mL) per day. Children are often receiving juice and other sweetened beverages outside of child care, therefore the Food and Beverage Criteria limit juice to no more than twice a week.
Sugar substitutes
Sugar substitutes include artificial sweeteners (e.g. acesulfame-potassium, aspartame, erythritol, neotame, sucralose, thaumatin) and sugar alcohols (e.g. sorbitol, isolmalt, lactitol, maltitol, mannitol and xylitol). Sugar substitutes are used to lower sugar and calorie content of food and beverages such as sweetened beverages, yogurts, sodas, cookies and many other foods.
Children have small appetites. If they eat foods with sugar substitutes regularly, they may not get the nutrients and energy they need for healthy growth and development. This is particularly the case with artificially sweetened beverages, which are low in nutritional value and often replace more nutrient dense beverages such as milk. For these reasons, avoid sugar substitutes.
Portion sizes
Canada’s Food Guide is intended for individuals two years of age and older. The foods served between six months and two years should include a variety of foods from Canada’s Food Guide, so that by the time toddlers are two years old, they are consuming a variety of foods along with the other children.
Children have small stomachs that fill quickly. Small, frequent, nutritious and energy- dense meals and snacks, including a variety of foods from the four food groups
are recommended to meet the nutrient and energy needs of infants, toddlers and young children.
The amount of food consumed by a child will vary from day to day and from child to child. Generally the size of a portion increases with age. For example, a two-year-old may eat a half slice of bread, whereas a four-year-old is more likely to eat a whole slice.
However, this can change based on the child’s appetite, growth spurts, how the child is feeling, distraction in the room, etc. When preparing foods it is important that you
offer each child sufficient foods and let the children determine how much they are going to consume.
A Food Guide Serving (FGS) is a reference amount. It is not intended to necessarily represent what someone would eat at one time, but it can be used as a consistent measure to compare how much people eat with the recommendations in Canada’s Food Guide. Children may not eat a full serving of Canada’s Food Guide or may they eat more than 1 serving from a food group. A guideline to follow is to offer children ½ of the Food Guide Serving for each food group and provide more food if children are still hungry.
Processed foods
Children’s nutrition needs are different from adults. They have small stomachs and require frequent nutrient dense meals. A focus on healthy foods, prepared with little to no added fat, sugar and salt, will help ensure they meet their nutrient needs. These healthy foods are whole foods or minimally processed and nutrient dense. Offering foods that are not nutrient dense could mean that a child may not receive their nutrition requirements.
Menus should focus on foods that are fresh and/or minimally processed with little to no additives or preservatives. The more a food is processed, the more nutrients that are lost. When foods are prepared from a recipe with whole ingredients, the ingredients can be modified or reduced to control the amount of added fat, sugar and salt. In addition to reducing fat, sugar and salt, healthy ingredient substitutions can also increase the nutrients available in the foods (e.g. fibre and calcium).
Resources to Explore
- Do Canadian Children Meet Their Nutrient Requirements Through Food Intake Alone?
- Healthy Teeth for Children
- The Use and Misuse of Fruit Juice in Pediatrics
- The Safety of Sugar Substitutes
- Alberta Nutrition Guidelines For Children and Youth: A Childcare, School and Recreation/Community Centre Resource Manual
Healthy Substitutions
Cooking: Improve the nutritional value and lower the amount of fat, sugar and salt.
| Use less fat | |
| Instead of | Try |
| Frying | Grilling, baking, roasting, broiling, or poaching |
| Butter, margarine, or oil in the amount called for
|
Using less than the recipe calls for |
| Replacing with cooking spray, water, or broth, or using a non-stick frying pan | |
| Fatty cuts of beef, pork, lamb, or sausage | Lean cuts of meat such as “loin” or “round”, and trimming visible fat |
| Fish, dried peas, beans, or lentils | |
| Cooking poultry with skin on
|
Removing the skin and excess fat |
| Adding colour with paprika, herbs, or tomato sauce | |
| Ground beef or pork in hamburgers, meatloaf, meat balls, etc. | Adding it raw and cooking until tender in the liquid, or browning in a non-stick skillet or one that has been sprayed with a non-stick cooking spray |
| Browning meat in oil or other fat for a stew or sauce | Adding it raw and cooking until tender in the liquid, or browning in a non-stick skillet or one that has been sprayed with a non-stick cooking spray |
| Cream
|
Using skim,1% or 2% milk, or evaporated milk or equal parts of low-fat milk and evaporated milk |
| Using fortified milk (one part skim milk powder to four parts low-fat or skim milk) | |
| Using low-fat sour cream | |
| Full-fat cream cheese | Using fat-free or low-fat cream cheese, yogurt cheese, or cottage cheese puréed until smooth |
| Full-fat sour cream | Replacing all or part with fat-free or low-fat sour cream, cottage cheese, part skim ricotta, yogurt cheese, or plain yogurt (250 mL yogurt blended with 15mL cornstarch if it will be cooked) |
| Use less sugar | |
| Instead of | Try |
| Fruit canned in syrup | Using fresh fruit or fruit canned in its own juice or water |
| Syrup | Using puréed fruit or small amounts of syrup |
| Using the suggestions in Healthy Substitutions – Baking | |
| High-sugar baked goods | Lean cuts of meat such as “loin” or “round”, and trimming visible fat |
| Fish, dried peas, beans, or lentils | |
| Use less sodium | |
| Instead of | Try |
| Canned broth | Using homemade stock, or commercial reduced sodium or salt-free stock, or bouillon in soups, gravies, sauces, dressings, etc. |
| Regular canned foods | Using foods canned in water, preferably with no salt added |
| Using reduced-sodium products | |
| Draining and rinsing canned foods for 30 seconds | |
| Using fresh foods when possible | |
| Processed, cured, or smoked meats | Using fresh or frozen meat or poultry cooked without salt or high-sodium smoked meats ingredients |
| Instant packaged foods, especially with salty powder or sauce packets | Preparing product from scratch using fresh ingredients |
| Using only a small amount of the prepared powder or sauce | |
| Using homemade herb and spice mixtures | |
| Using chopped or sliced vegetables or fruit instead of pickles | |
| Using homemade chunky fruit or vegetable sauces like salsa, chutney or relish | |
| Commercial condiments | Using small amounts (1 tsp (5 mL) to 1 tbsp (15 mL)) of condiments such as ketchup, soy sauce, commercial salad dressings and salsas, etc. |
| Substituting reduced-sodium products | |
Baking: Improve the nutritional value and lower the amount of fat, salt and sugar.
| Boost fibre | |
| Instead of | Try |
| 250 mL white flour | Using 125 mL white flour plus 125 mL whole wheat or whole grain flour |
| Using 175 mL white flour plus 50 mL ground flaxseed | |
| Adding wheat bran or oatmeal to breads and muffins | |
| Use less fat | |
| Instead of | Try |
| 125 mL fat (e.g. oil, margarine or butter) | Using 50 mL mashed fruit plus 50 mL fat; use applesauce, apple butter, mashed banana, puréed prunes or puréed pumpkin (using mashed fruit may reduce the baking time by 25%) |
| 250 mL fat (e.g. oil, margarine or butter) | Using 150 to 175 mL fat |
| 250 mL solid fat (e.g. margarine, butter, or shortening in yeast breads) | Using 175 mL ricotta cheese plus 50 mL solid fat |
| Cream | Using low-fat evaporated milk, or low-fat sour cream |
| Use less salt | |
| Instead of | Try |
| Using the amount called for | Omitting the salt or using less |
| Use less sugar | |
| Instead of | Try |
| 250 mL sugar | Using 150 to 175 mL sugar; add cinnamon, vanilla, or almond extract |
| 250 mL chocolate chips | Using 125 to 250 mL chopped nuts or chopped dried fruits such as cranberries, raisins, apricots or cherries (or a combination) |
| Fruit canned in syrup | Using fruit canned in its own juice or water, or fresh fruit |
| Frosting or icing | Using sliced fresh fruit, or puréed fruit |
| Boost iron | |
| Instead of | Try |
| 125 mL fat (e.g. oil, margarine or butter) | Using 50 mL fat plus 50 mL pumpkin purée |
| Adding raisins, dried apricots, pumpkin or sesame seeds, nuts, oatmeal, wheat germ | |
| 375 mL sugar in breads, muffins cookies | Using 250 mL blackstrap molasses and 175 mL sugar; add 2 mL of baking for each 250 mL molasses; omit baking powder or use half the amount. Molasses should not replace more than half of the sugar called for in a recipe |
Infant Feeding Plans
Infant Feeding Plans are developed at the request of parents or when foods from home are provided for children between birth and 17 months old. The following is a list of possible questions that may be used when developing an infant feeding plan:
- What types of food does the child currently consume?
- Have solid foods been successfully introduced, and, if so, what types?
- What textures have been successfully introduced?
- What are the child’s food preferences?
- What are the child’s self-feeding abilities?
- Are there any dietary considerations or special requests?
- Does the child have any identified allergies, food intolerances or any suspected concerns?
- What are the child’s feeding times/routines?
- Are there any foods that the parents wish to wait to introduce?
- What is the plan for updating and making changes to a feeding plan?
- To what extent will the child care setting be involved in introducing new solids/textures?
- What is the plan for breast milk supply (e.g. liquid or frozen)?
- How should the child care setting respond in the event that breast milk is unavailable (e.g. runs out)?
- May the child eat modified items from menu?
- Are there any food requests based on medical issues?
- Will the child consume food from home as well as from the center? If so, how should the child care setting respond in the event that foods and beverages brought from home are unavailable (e.g. run out)?
These questions may be helpful when developing an Infant Feeding Plan. Infant Feeding Plans are especially beneficial to ensure there is ongoing communication between the child care setting and the family.
Feeding plans may be created for infants (children between the ages of birth to 17 months) upon enrolment in a regulated child care setting at the request of parents or when the parent requests that foods be supplied form home. This will enable ongoing communication between the infant’s parent/guardian and the care provider or the child care staff, including the cook and can be used in conjunction with the infant daily record.
Name of Child:
Date of Birth:
Age at time of enrolment:
| Does your child currently consume | Feeding method | Special instructions |
| Breastmilk, formula, solid foods** | Breastfed, bottle, spoon, cup | This can include: breastmilk or formula storage and supply, food allergies, religious/cultural food requests, food requests related to medical conditions etc. This can also include if the infant will consume food from home at the parents’/guardians’ request, or consume the foods served in the centre. |
| Solid foods that have been introduced | Feeding abilities (e.g. fed by caregiver, self feed with fingers, spoon and/or fork) | |
| Textures (e.g. pureed, minced, diced) |
* Regulated child care settings welcome mothers to breastfeed anywhere in the facility or home. Ongoing communication between centre staff and the parent/guardian will occur to make sure there is an adequate supply of your breastmilk for your child at the centre. No other form of nutrition will be provided unless instructed by the parent/guardian.
** It is important that infants receive nutrient dense, iron containing foods at 6 months of age. This may include foods from the Meat and Alternative group, including meats, fish, poultry, cooked egg yolks, tofu and well-cooked legumes.
Chapter Attribution
Chapter adapted from: Government of Nova Scotia. (2011). Manual for Food and Nutrition in Regulated Child Care Settings: Section A. https://www.novascotia.ca/coms/families/provider/documents/manual-food_and_nutrition.pdf

