23 Communicable Diseases
Learning Objectives
After reading this chapter you will:
- Be familiar with practices to reduce the spread of infections and communicable diseases in a child care setting.
- Understand why the preventive practices are important.
Hand Washing
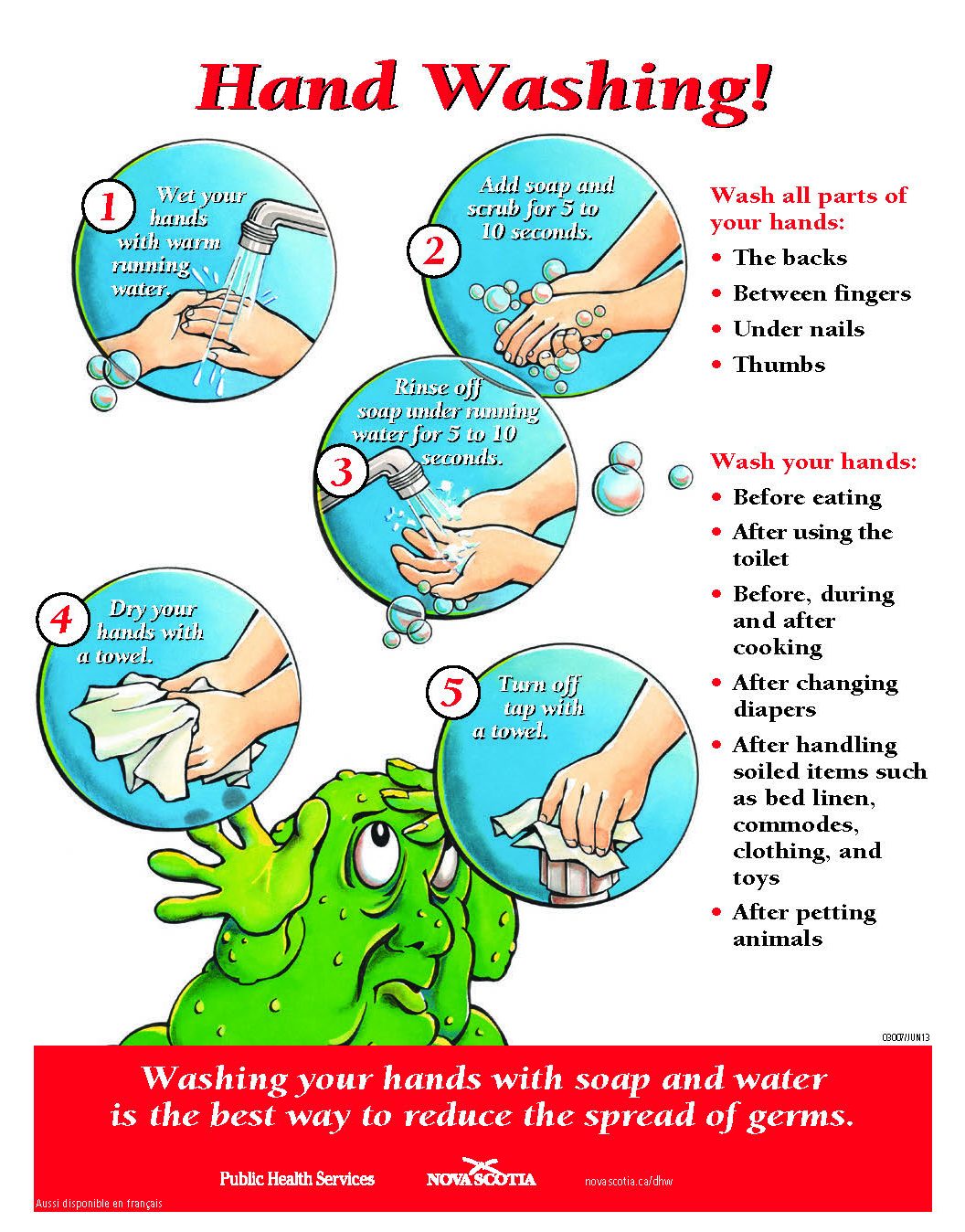
Hand washing is the single most effective way to prevent infections from spreading. Enforcing proper hand washing by staff, food handlers, and children helps ensure a safe and healthy environment. The best kind of sink for hand washing has hot and cold water mixed through one faucet, and also has foot, knee, or wrist-operated water controls. Mixing valves maybe required.
Supply the hand wash sink with paper towels and liquid soap in a dispenser. It is not necessary to use disinfectant or antimicrobial soaps. Cartridge-type dispensers, rather than refillable soap dispensers, are preferable. If you use refillable liquid soap dispensers, clean and sanitize the containers before refilling them. Cloth towels are not recommended. For an illustration of the proper hand washing technique refer to Proper Hand Washing Procedures poster.
Alcohol-based hand rubs should only be used when soap and water are unavailable. It is recommended that alcohol-based hand sanitizers have a minimum of 60 per cent ethanol (ethyl alcohol). Hand sanitizers should not be used if hands are visibly soiled with dirt or other contaminated material (e.g., stool, urine, vomit or blood). Children must be supervised while using alcohol hand rubs because it can be harmful to the child, if swallowed. Allow the hands to dry completely before children touch anything, especially before hand-to-mouth contact. These products should be stored away from children.
Diapering
The rate of intestinal infection in programs directly relates to the presence of children in diapers. Diaper changing is one of the highest risk procedures for the spread of diarrhea illness among children and staff. Proper hand washing, cleaning and disinfecting of diaper change tables help prevent diarrheal illness in the program.
To help reduce the spread of intestinal illnesses, the program must ensure there is a
- properly designed diaper change area
- proper procedure for using gloves
- proper procedure for changing diapers
- proper procedure for toileting
Diaper Change Area Guidelines
When designing a diaper change area, follow these guidelines:
- Always separate diaper change areas from food preparation areas. Diaper change areas require a separate hand washing sink with liquid soap and paper towel.
- Always ensure the diaper change table and pad is made of a smooth, non-absorbent, and easily cleanable material. Clean and disinfect the diaper change table in between each diaper change.
- Always make sure the waste container has a tight-fitting, foot-operated lid and is lined with a disposable plastic bag. Empty the container frequently. Clean and disinfect it at least daily.
- Never dispense creams and ointments in a way that contaminates the contents, such as with fingers, common sticks, or tissues. If special creams are necessary ALWAYS use an individual utensil to dispense it for each child.
- Never rinse soiled clothing or cloth diapers at the program. Place soiled clothing or cloth diapers in a sealed plastic bag for home washing.
- Never use just hand sanitizer between diaper changes—wash your hands with soap and water.
Food Safety Practices
Children must receive food that is safe and healthy to eat. Safe food helps prevent the development and spread of infectious illnesses, such as gastroenteritis.
Proper food safety requires that staff and food service staff practice good personal hygiene and know how to handle food safely when preparing, storing, and serving it.
All programs serving meals must have at least one person who has successfully completed a recognized food handlers training course present in the food preparation area at all times when food is being prepared. Information on these courses can be found by visiting Food Hygiene (Handling) Courses on the NS Department of Environment and Climate Change web page.
Personal Hygiene
To practice good personal hygiene, follow these steps:
- Develop and enforce a clear policy about staff and illness. For example, no food handler may work while suffering from a gastrointestinal illness such as diarrhea.
- Ensure that food handlers wash their hands with liquid soap and warm water
-
- before starting work
- upon return to work from a break
- after using the washroom
- after handling raw meats, vegetables or fruits
- after handling garbage or garbage containers
- after blowing or wiping their nose
- after completing any other activity that may have contaminated their hands
- Ensure that food handlers have clean hands, clothes, and hair restraints. Do not allow smoking in the kitchen or on the premises of the program.
- Ensure that staff who change diapers wash their hands both after diapering and before preparing food.
Food
Receiving, storing, preparing and handling food properly are essential in ensuring the program serves safe food. To safely prepare food follow these guidelines:
Thawing Food
- Do not thaw food on a counter at room temperature. This can cause rapid bacterial growth and can result in food poisoning.
- Practice the following safe thawing methods:
- Thaw food in a refrigerator.
- Thaw food under cold running water, if rapid thawing is necessary.
- Thaw food in a microwave and then cook immediately.
- Cook from frozen where applicable.
Preparing Food
- Thoroughly wash all raw fruits and vegetables under cold running water.
- Wash the tops of canned food before opening. Wash the opener with clean, soapy water after each use.
- Avoid hand contact with food by using clean utensils to mix and serve food.
- Before each use, clean and sanitize all utensils you use to taste food during preparation. Do not put a utensil you just used to taste food back into a pot or dish that contains food that will be served to others.
- Clean and sanitize all surfaces as you prepare the food to prevent cross contamination of food and work surfaces. Where possible, use separate areas or utensils for raw and ready-to-eat foods.
- Clean and sanitize work areas and wash your hands when changing from raw to cooked food, or from raw to ready-to-eat food.
- Ensure a minimum internal temperature of 74°C (165°F) when cooking food, or 82°C (180°F) when cooking whole poultry. For more details please see Food Safety Factsheet.
- Maintain a minimum temperature of 60°C (140°F) when holding hot food.
- Ensure a minimum internal temperature of 74°C (165°F) when reheating food.
- Refrigerate prepared food as quickly as possible. The prepared food should be no deeper than two inches (approximately 5 cm), to enhance rapid cooling.
- Dispose of leftover food that has been put out in serving bowls for the children.
Breast Milk
Breast milk is the only food an infant needs for the first 6 months of life. If an infant is not breastfed, formula is the only acceptable substitute for the first 6 months of life. Infants should not be fed solid food before 6 months. Breast milk will continue to be the infant’s main source of nourishment for 12 months, and continue to provide nourishment for as long as the mother continues to provide breast milk.
Some mothers may switch between breast milk and formula, or feed their baby both as needed. It is important to work with the family to develop an infant feeding plan to address feeding and storage of breast milk. This may also include a plan to follow if the supply runs out, and a ‘transition’ plan to other milks if/when necessary.
To safely store breast milk:
- Ensure bottles and containers are labelled with the following:
- child’s name
- date received
- date to be used by
- Store the breast milk in the refrigerator or freezer as soon as it is received, as requested by the family. Breast milk may be stored in the same fridge as other foods.
- Never leave freshly expressed breast milk at room temperature for more than 3-4 hours.
- Breast milk that has not been previously frozen can be stored in the refrigerator between 0°C (32°F) and 4°C (40°F) for up to 5 days, however less than 72 hours is ideal.
- Breast milk that has been frozen can be stored for different lengths of time depending on the type of freezer.
- In a freezer compartment inside a refrigerator at a temperature of -15°C (5°F) for 2 weeks
- In a freezer compartment with a separate door at a temperature of -18°C (0°F) for 3-6 months
- In a deep freeze at a temperature of -20°C (-4°F) for 6–12 months
- Previously frozen breast milk that has been thawed can be safely kept refrigerated for up to 24 hours, after which it should be discarded.
To safely prepare breast milk:
- Wash your hands before and after preparing breast milk and handling bottles.
- Clean and sanitize counters where bottles of breast milk are prepared.
- Frozen breast milk can be thawed in the refrigerator or by placing the container in lukewarm water.
- To warm breast milk, place the container or bottle in a pan or bowl of warm water.
- Do not heat breast milk in the microwave. Microwaves cause uneven heating and the breast milk could scald the infant.
To safely feed breast milk:
- Wash your hands prior to and after feeding.
- An infant must not be fed in a crib or by bottle propping. An infant who cannot hold a bottle must be held by staff during the feeding.
- If the baby does not finish the breast milk bottle, it may be used again within 1–2 hours. If not used within 1–2 hours, it must be discarded.
- If a child is given the breast milk intended for another child, the family of both the children must be notified.
Formula
For infants who are not breastfed, formula is the only food an infant needs in the first 6 months of life. Infants should not be fed solid food before 6 months. Formula will continue to be the infant’s main source of nourishment from 6–12 months of age. Some mothers may switch between breast milk and formula, or feed both as needed. Work with the family to develop an infant feeding plan to address feeding and storage of formula. This may also include a plan to follow if the supply runs out, and a ‘transition’ plan to other milks if/when necessary.
Formula is available in ready-to-serve liquid, a concentrated liquid, or a powder form. It is important to follow the measuring directions on the formula container exactly.
To safely store formula prepared at home:
- Ensure bottles and containers of formula are labelled with:
- child’s name
- date prepared
- date received
- date to be used by
- Store prepared formula in the fridge as soon as it is received. Prepared formula may be stored in the same fridge as other foods.
- Never leave prepared formula (powdered, liquid concentrate, or ready to serve) at room temperature for more than 2 hours.
To safely feed prepared formula:
- Wash hands prior to and after feeding.
- Do not heat infant formula in a microwave. Microwaves cause uneven heating and the formula could scald the infant.
- Leftover formula must be discarded. Infants must start a new bottle at each feeding.
- An infant must not be fed in a crib or by bottle propping. An infant who cannot hold a bottle must be held by staff during the feeding.
- If a child is given the formula intended for another child, the families of both the children must be notified.
When formula is prepared in a program the following guidelines should be followed:
For ready-to-serve liquid formula:
- Ready-to use formula does not need to be mixed.
- Wash your hands prior to preparing formula.
- Until a child is 6 months old, everything used to prepare the formula needs to be sterilized each time by boiling for 2 minutes to make sure it is germ-free. This includes things like the measuring cup, can opener and tongs, as well as bottles and nipples.
- After a child is 6 months old, everything used to prepare the formula must be washed and sanitized as per the Nova Scotia Food Retail & Food Services Code
- Clean and sanitize counters where formula is prepared.
- Store the filled bottles in the refrigerator. The bottles must be used within 48 hours. After this the formula must be discarded.
- Once opened, ready-to-use formula can be covered and stored in the refrigerator for up to 48 hours. After this it must be discarded.
For liquid concentrate formula:
- Wash your hands prior to preparing formula.
- Until a child is 6 months old, everything used to prepare the formula needs to be sterilized each time by boiling for 2 minutes to make sure it is germ-free. This includes things such as the measuring cup, can opener and tongs, as well as bottles and nipples.
- After a child is 6 months old, everything used to prepare the formula must be washed and sanitized as per the Nova Scotia Food Retail & Food Services Code
- Clean and sanitize counters where formula is prepared.
- Until a child is 6 months old, all types of water used to prepare the liquid concentrate formula must be boiled for at least 1 minute and cooled before mixing.
- Well water must be tested for bacteria and chemical content. It is not safe to use well water that has high levels of chemicals or minerals to mix formula, even if you boil it.
- The Nova Scotia Department of Environment recommends that your well water be tested every 6 months for bacteria and every 2 years for chemical content.
- If well water is used, continue to use boiled water for as long as the baby drinks formula.
- To prepare the formula, follow the instructions on the can. Use a measuring cup, not a bottle, to measure liquids because the measurements on bottles are not always accurate.
- Store the filled bottles in the refrigerator at 4°C (40°F) or lower. The bottles must be used within 48 hours. After this the formula must be discarded.
- Once opened, the liquid concentrate formula can be covered tightly and stored in the refrigerator for up to 48 hours. After this, it must be discarded.
For powdered formula:
- It is not safe to use powdered formula for babies less than 2 months old.
- Wash your hands prior to preparing formula.
- Clean and sanitize counters where formula is prepared.
- Until a child is 6 months old, everything used to prepare the formula needs to be sterilized each time by boiling for 2 minutes to make sure it is germ-free. This includes things such as the measuring cup, can opener and tongs, as well as bottles and nipples.
- After a child is 6 months old, everything used to prepare the formula must be washed and sanitized as per the Nova Scotia Food Retail & Food Services Code.
- Well water must be tested for bacteria and chemical content. It is not safe to use well water that has high levels of chemicals or minerals to mix formula, even if you boil it.
- The Nova Scotia Department of Environment recommends that your well water be tested every 6 months for bacteria and every 2 years for chemical content.
- It is safest to prepare only one bottle of formula at a time because powdered formula cannot be sterilized and may contain a small amount of bacteria.
- To prepare the formula, follow the instructions on the can. Use a measuring cup, not a bottle, to measure liquids because the measurements on bottles are not always accurate.
- Regardless of infant’s age, all types of water used to prepare the powdered formula must be brought to a rolling boil for 1 minute and cooled to no less than 70°C (158°F) (cool for no more than 30 minutes at room temperature) before adding powder. The prepared bottle of formula may then be cooled to room or body temperature (37°C) by quickly placing the bottle under cold running water or into a container of cold or ice water prior to feeding the infant to avoid potential scalding.
- If preparing formula for later use, the water used to prepare the formula must be brought to a rolling boil for 1 minute, dispensed into containers of a maximum size of 1 L and cooled down to no less than 70°C (158°F) (cool for no more than 30 minutes at room temperature) before adding powder. The prepared bottle of formula may then be cooled to room or body temperature (37°C) by quickly placing the bottle under cold running water or into a container of cold or ice water prior to feeding the infant to avoid potential scalding.
- If well water is used, continue to use boiled water for as long as the baby drinks formula.
- If not used immediately, put the filled, cooled bottles in the refrigerator right away.
- Formula that is prepared for later use can be stored up to 24 hours when refrigerated at 4°C (40°F).
- Store open containers of powdered formula in the original container with a tight-fitting lid in a cool, dry area and off the floor.
- Store open cans of powdered formula for up to 30 days only. Label each can with the date it was opened. Discard after 30 days or before the expiry date, whichever comes first.
To safely feed prepared formula:
- Wash hands prior to and after feeding.
- Do not heat infant formula in a microwave. Microwaves cause uneven heating and the formula could scald the infant.
- Leftover formula must be discarded. Infants must start a new bottle at each feeding.
- An infant must not be fed in a crib or by bottle propping. An infant who cannot hold a bottle must be held by staff during the feeding.
- If a child is given the formula intended for another child, the families of both the children must be notified.
Preparing for Picnics and Outings
When planning for picnics and other outings, consider the duration of the outing and the availability of proper refrigeration. Improper storage of food increases the capability for bacterial growth and can result in an outbreak of food poisoning.
To properly prepare for picnics and outings, follow these guidelines:
- Bring only non-perishable foods, if possible. These are foods that do not support bacterial growth, i.e., normally do not require refrigeration to be kept safe.
- Keep perishable food, such as cooked meat, fish, poultry, and dairy products at a temperature less than 4°C (40°F). Do not bring raw meat, fish, or poultry on an outing.
- Use alcohol-based hand rubs or moist towelettes to clean hands of staff and children before eating, if proper hand washing facilities are not available.
- Drink water from a known safe source only. Do not drink from springs, streams, and similar sources. If uncertain, always bring bottled water.
Serving Catered Foods
Catering includes foods from local restaurants and food service providers. Preparing and storing food properly is important if the program uses catered food. The caterer must be able to answer several questions:
Where does the caterer prepare the food?
The food must be prepared in a licensed facility.
How does the caterer transport the food to the program?
The caterer must protect the food from contamination both during transportation to the program and upon arrival. The covered containers must either be disposable or made of an easily cleanable, non-absorbent, food-grade material.
What is the temperature of the food during transportation to the program and upon arrival?
The caterer must keep hot food at a temperature above 60°C (140°F) and cold food below 4°C (40°F).
WHAT utensils will the program use to serve and eat the food?
The caterer must supply an adequate number of clean, sanitized utensils. If the caterer does not supply utensils, the program must have them available as well as the ability to clean and sanitize them. The program must contact a Food Safety Specialist if the safety or integrity of the food is in question. To contact a Food Safety Specialist, please see: Department of Environment and Climate Change offices.
Food from Home
- Food brought in from homes may be a risk to food safety, because the means of preparation, cooking, temperature and transporting of these foods is not known.
- When medical or dietary needs require a child to bring food from home or if the child is in the school-aged program, this food must be labelled with the child’s name and refrigerated if required.
- Food considered to be a low-risk food by Nova Scotia Environment, including whole fruits and vegetables that have not been cut except for the purpose of harvesting and dry non-potentially hazardous baked goods (i.e., those that do not contain cream, custard, cream cheese, meat or any other potentially hazardous food as filling or a topping) may be brought into the program if this is acceptable to the licensee.
- For specific requirements related to food safety, please see the Food Safety Standard, page A15, in the Manual for Food and Nutrition in Regulated Child Care Settings
Storing Food
To provide children with safe and wholesome meals, the program must create and enforce proper conditions for storing food. To properly store food, follow these guidelines:
Refrigerated Foods
- Check that each refrigerated space has an accurate indicating thermometer.
- Store meats, fish, poultry, and dairy products at a temperature below 4°C (40°F). Store raw meats, fish, and poultry on the lowest shelf with all cooked ready-to-eat foods stored above.
- Keep frozen food at a temperature below -18°C (0°F).
- Follow the manufacturer’s label for storage requirements of other food products.
- Cover or wrap and label all food in refrigerators and freezers—label with the food name, date, and the cook’s name.
- Ensure adequate air circulation for even cooling. Do not overstock refrigerators, which could block or prevent air circulation.
- Store raw perishable foods for 2 to 3 days only. Consider freezing if longer storing time is required.
Dry Storage (non-refrigerated food)
- Keep storage areas clean, dry, well-ventilated, and adequately lit.
- Store only food in food storage areas.
- Store food at least 15 cm (6 inches) above the floor on racks or pallets.
- Check that all shelving is made of easily cleanable and non-absorbent material.
- Place open package and bulk foods in sealed and easily cleanable containers to prevent contamination.
- Store insecticides and chemicals in a locked cupboard or room away from food and children.
Cleaning and Sanitizing Utensils
Dirty utensils can contaminate food. The improper cleaning and sanitizing of utensils can result in unsafe food. Unsafe food can in turn lead to food poisoning. Clean and sanitize all utensils that touch food before using them. Avoid cross contamination—do not use a knife to cut raw chicken and the same knife to cut cooked chicken. Properly wash the knife between uses. A safe method to clean and sanitize multi-service utensils should include either a three-compartment sink or a dishwasher.
Environmental Sanitation
Many germs that can cause illnesses survive for a long time on surfaces. Some germs only live for a few hours, while others can live for several days or even weeks. In some cases, it only takes a few germs to cause an illness. Proper cleaning and disinfecting practices play an important part in preventing illnesses and infections in the program. To have a clean, safe environment, the program must develop and enforce proper cleaning and disinfection policies.
Cleaning
Cleaning is an important way to remove visible dirt from various surfaces. To remove dirt, rub the surface with a cloth or towel moistened with a household detergent. The rubbing action creates friction and the detergent helps break down fats and proteins.
Cleaning removes some germs from a dirty surface, but does not necessarily remove all of the germs. Certain germs are very resistant to detergents. The only way to remove them is to sanitize the surface properly.
A good way to remember the difference between cleaning and sanitizing is that cleaning gets rid of the dirt you can see, while sanitizing gets rid of most of the germs you can’t see.
Sanitizing
Sanitizing reduces the germs present on a surface or object. Sanitizing should not be done on its own. Always clean before sanitizing as dirt places a great demand on the chemical found in sanitizing solutions and reduces their effectiveness. If sanitizing is done without cleaning, the surface may not be properly sanitized. Use rubber gloves when sanitizing to avoid contact with corrosive materials that cause skin problems. Always wash hands after cleaning or sanitizing. Wash hands immediately after removing rubber gloves.
Disinfecting
Disinfection inactivates or kills the germs that may be present on environmental surfaces and that cleaning does not remove. Always clean before disinfecting. Use rubber gloves when disinfecting to avoid contact with corrosive materials that cause skin problems. Always wash hands after cleaning or disinfecting. Wash hands immediately after removing rubber gloves.
Mixing a Disinfectant Solution
Household bleach is the most commonly used chemical for disinfecting objects and surfaces in programs. It is convenient, readily available, economical, and effective. Undiluted bleach is a corrosive chemical. It is important to dilute it to a working strength. There are a number of other disinfectant and sanitizing products available that are suitable for use in programs. Alternative products to bleach can be used provided that:
- The product has a drug identification number (DIN) for food contact surfaces and pest control product (PCP) registration number for non-food contact surfaces on the label.
- It is effective for its intended use.
- The manufacturer’s directions can be followed exactly as printed on the label.
Instructions for Mixing Various Disinfectant Solutions
|
Household Bleach (Original strength approx. 5.25% sodium hypochlorite) |
||
| To Disinfect/Sanitize | Dilution | Method |
| Bathrooms, diaper change tables, toys, water tables, sleep mats, chairs, general surfaces | Mix 2 teaspoons (10 mL) of bleach to each litre of water. Approximately 500 parts per million (ppm) chlorine | Apply to a cleaned surface and leave on the surface for 2 minutes. Allow to air dry. Surfaces such as diaper change tables and potties can be wiped dry after 30 seconds with a clean, single-use paper towel |
| Food contact surfaces, dishes, eating utensils, toys that children put in their mouths | Mix ½ tsp (2.5 mL) – 1 tsp (5 mL) of bleach to each litre of water. Approximately 100 ppm of chlorine | Immerse cleaned object in sanitizer solution for 2 minutes or spray on surfaces and allow to stand for at least 2 minutes. Surface may be wiped with a clean, single-use paper towel |
| Surfaces contaminated with blood, feces, vomit, or other bodily fluids | Mix 7 tablespoons (Tbsp) (100 mL) of bleach to each litre of water. Approximately 5000 ppm of chlorine | Apply to a cleaned surface and leave on the surface for 30 seconds. Allow to air dry. Adequate ventilation must be provided. |
| Using Quaternary Ammonia Compounds | ||
| To Disinfect/Sanitize | Dilution | Method |
| Food contact surfaces, dishes, eating utensils, toys that children put in their mouths | 200 ppm | Follow manufacturer’s instructions |
| Using Iodine | ||
| Food contact surfaces, dishes, eating utensils, toys that children put in their mouths | 25 ppm | Follow manufacturer’s instructions |
Directions for mixing disinfectant/sanitizer solutions
- Use only potable (drinkable) water.
- Always pour bleach into water.
- Do not use clear spray bottles or containers because light quickly weakens the strength of the solution.
- Mix a fresh solution daily. Household bleach solutions quickly lose strength. Discard unused/leftover solutions at the end of the day.
- Label containers with the name of the solution and its dilution. Follow the requirements of your Workplace Hazardous Materials Information System (WHMIS) program for the labeling and storage of sanitizers.
- For all other sanitizers or disinfectants, follow the manufacturer’s instructions for application strength, contact time and rinsing or wiping.
- DO NOT mix bleach with any other chemicals.
- Keep all chemical solutions out of children’s reach.
Clothing
Personal clothing and other items must be stored in individual cubicles (cubbyholes) or on hooks. Personal clothing and items including cloth diapers that have been soiled must not be rinsed in the program and must be placed in a sealed plastic bag to be washed at home. Wash dress-up clothing each week or more often if soiled.
Furniture and Equipment
To properly sanitize certain furniture and equipment, spray tables and chairs with the sanitizing solution and let the solution sit for at least 2 minutes. Wipe dry with a clean, single-use towel.
Toys
Clean and sanitize infant and toddler mouth toys at least once a day. Clean and sanitize other toys and toys used by older children once a week, or more often if contaminated.
To properly clean and sanitize toys to prevent the spread of germs, follow these guidelines:
- Wash and sanitize plastic toys as you would for furniture and equipment as discussed above.
- Moist-wipe toys such as books and puzzles with a sanitizer each week.
- Launder soft, cuddly toys at least once a week and more often, as required.
- Store personal toys in the child’s cubicle when not in use.
- Personal toys including stuffed toys that have been soiled must be placed in a sealed plastic bag to be washed at home.
Sandboxes, Water Play and other Sensory Play Areas
Sandboxes and water areas are great places for children to play, but they also are a source for germs. To establish safe play areas, follow these guidelines:
Outdoor Sandboxes
- Cover outdoor sandboxes when they are not in use to prevent access by animals. Check that the lid fits tightly.
- Rake the sand daily and inspect for animal or human feces or urine.
- If animal or human feces is found, empty the sandbox, discard the contaminated sand, clean and disinfect the sandbox, and allow to air dry before refilling it with clean sand.
- If only urine is present, leave the sandbox open to sunlight. Children should not be allowed to use it for 24–48 hours.
- Clean and disinfect sandbox toys at least once a week.
- Replace outdoor sand every 2 years.
Indoor Sandboxes
- Cover the sand table when not in use.
- Discard any sand that has fallen on the floor.
- Throw out the contents and clean and sanitize the sand table 3 times a year or more often if contaminated.
- Clean and disinfect sand table toys at least once a week.
Water Play Tables
- Both staff and children should wash their hands before and after water play.
- The water table should be filled with fresh potable water immediately before use.
- Supervise children and ensure they do not drink the water.
- Drain, clean, and disinfect water play container after each use—at least once a day.
- Clean and disinfect toys used in water play each day.
- Children who have an infection of any kind, or who have open sores or wounds, cannot participate in water play.
- During an outbreak, water play table use should be discontinued.
Wading Pools
- The wading pool should be filled with fresh potable water immediately before use.
- Wading pools should be stored to prevent water collecting in the pool.
- The wading pool must have a depth of less than 12 inches of water.
- Supervise children and ensure they do not drink the water.
- Empty, clean and disinfect the pool after each use.
- Children in diapers cannot participate in wading pool play.
- Children who have an infection of any kind, or who have open sores or wounds, cannot participate in water play.
- During an outbreak, wading pool use should be discontinued.
- Other Sensory Play Materials
- Both staff and children should wash their hands before and after sensory play.
- Sensory play items such as rice, pasta, confetti and others must be discarded once a week or more frequently if contaminated.
- Clean and disinfect the basin when the sensory material is changed.
- During an outbreak, sensory play table use should be discontinued.
Cots and Cribs
Sleeping areas also are a potential source for spreading illnesses. To prevent spreading illnesses, follow these guidelines:
- Assign each crib, cot, or sleeping mat and appropriate linen to a specific child.
- When in use, separate cribs, cots or sleeping mats by at least 46 cm (18 in.), so that children are not able to touch each other. See Early Learning and Child Care Regulations.
- Ensure each child’s linen is separated during storage.
- Store sleeping mats or mattresses (including linen) that are placed directly on the floor in separate plastic bags.
- Launder all linen each week.
- Launder linen and clean and disinfect cots, cribs, crib mattresses, or sleeping mats contaminated with feces, urine, or other bodily fluids immediately and before assigning to another child.
Washrooms
Proper cleaning and sanitizing is crucial in washroom areas to avoid spreading illnesses.
To properly clean and disinfect the washroom, follow these guidelines:
- Wear gloves as a personal protection from cleaners.
- Clean and disinfect the washroom including faucets, sinks, and toilet seats at least once each day, and more often as necessary.
- Start from the highest areas and move to the lowest areas—from the ceiling down
to the floors. This way, you work on the least soiled areas first and the most soiled areas last. - Ensure adequate supplies of toilet paper, liquid soap, and paper towels in dispensers.
- Proper Procedure for Using Disposable Gloves
You should wear disposable gloves when there is the chance of infection transferring to you during care activities. This is especially important when the child has diarrhea. However, it is good practice to always use disposable gloves during diaper changing. If you wear disposable, single-use gloves remember a few very important rules. You must:
- Never use gloves as a substitute for hand washing.
- Wash your hands after wearing gloves.
- Wear gloves on both hands.
- Wear a new pair of clean gloves to perform caregiving activities for each child.
- Remove gloves and wash your hands when going from a ‘dirty’ to a ‘clean’ procedure (e.g., from changing diapers—a dirty procedure—to helping wash the child’s hands—a clean procedure).
Proper Procedure for Changing Diapers
To establish a proper diaper changing procedure, you should:
- Wash your hands with soap and water before each diaper change; do not use just hand sanitizer between changes.
- Assemble all necessary supplies before starting (e.g., fresh diapers or clothes, towelettes and/or paper towels).
- Hold the child away from your body and place the child on a clean table or change pad and remove the dirty diaper. Fold the diaper surface inward and set it aside. Never place safety pins in your mouth or within reach of the child.
- Clean the child’s skin with a moist disposable cloth or towelette, wiping the child’s bottom from front to back. Remember to wash in the creases in the child’s skin.
- Diaper and dress the child.
- When cloth diapers are used, flush formed stool down the toilet (avoid splashing).
- Throw out disposable diapers and towelettes in the plastic-lined waste container. Place cloth diapers in a covered, lined diaper pail. DO NOT RINSE CLOTH DIAPERS.
- Wash your hands.
- Clean the change table/pad and spray a disinfection solution (1:100 household bleach) over the entire surface of the diaper change table after each use. Let the spray sit for a minimum of 2 minutes or follow the manufacturer’s instructions for dilution and contact time if using another disinfectant.
- Once the sanitizer has had contact time of 2 minutes, dry the change table surface with single-use paper towels and throw them out.
- WASH YOUR HANDS AGAIN THOROUGHLY.
- Record unusual skin conditions or bowel movements.
Proper Procedure for Toileting Using a Toilet
To develop a proper toileting procedure for toddlers, you should follow these steps:
- Remove the diaper.
- Place the toddler on the toilet.
- Wipe the toddler’s bottom from front to back and teach the toddler to do the same. This reduces the chance of urinary tract contamination.
- Flush the toilet or allow the toddler to flush it.
- Diaper and help dress the toddler as necessary.
- Help wash the toddler’s hands.
- If soiled, clean the toilet seat or toilet trainer seat and spray a disinfectant (1: 100 household bleach solution) over the entire surface of the seat. Let the spray sit for at least two minutes or follow the manufacturer’s instructions for dilution and contact time if using another disinfectant.
- Remove and throw out gloves and wash your hands.
- Once the sanitizer has had contact time for two minutes, dry the toilet seat or toilet trainer seat with single-use towels and throw them out.
- Wash your hands thoroughly.
- Record unusual skin conditions or bowel movements.
Proper Procedure for Toileting Using a Potty
To develop a proper toileting procedure for toddlers, you should follow these
steps:
- Remove the diaper.
- Place the toddler on the potty.
- Wipe the toddler’s bottom from front to back and teach the toddler to do the same. This reduces the chance of urinary tract contamination.
- Diaper and help dress the toddler as necessary.
- Help wash the toddler’s hands.
- Rinse the potty and flush contents down the toilet.
- Wear gloves and use toilet paper to remove remaining stool.
- Clean the potty and spray a disinfectant (1: 100 household bleach solution) over the potty’s entire surface. Let the spray sit for at least 2 minutes or follow the manufacturer’s instructions for dilution and contact time if using another disinfectant.
- Remove and throw out gloves and wash your hands.
- Once the sanitizer has contact time for 2 minutes, dry the potty with single use towels and throw them out.
- Return the potty to storage.
- Wash your hands thoroughly.
- Record unusual skin conditions or bowel movements.
Image Credits
The Communicable Disease Prevention and Control Division, Public Health Branch, Department of Health and Wellness [DHW]. (2013). Proper Hand Washing Procedures Poster. https://novascotia.ca/dhw/CDPC/documents/Guidelines_CDPC_Child_care_Setting.pdf
Chapter Attribution
Adapted from Province of Nova Scotia. (2015). Guidelines for Communicable Disease Prevention and Control for Child Care Settings (pp 20-37). https://novascotia.ca/dhw/CDPC/documents/Guidelines_CDPC_Child_care_Setting.pdf

