19.4 Theoretical Perspectives on Health and Medicine
Each of the three major sociological perspectives approaches the topics of health, illness, and medicine differently.
Positivist Sociology and Functionalism
Positivist approaches that seek to explain health outcomes from a sociological framework developed social epidemiology and the social determinants of health model, which predict health outcomes from background variables such as income, education, racialization, and other indicators of socioeconomic status. The Whitehall study in Britain in the 1960s was one of the first large scale empirical studies that indicated that inequality itself was a direct factor in determining a gradient of health outcomes (Marmot et. al., 1978). In a study of 17, 350 British civil servants, it was found that differences in even relatively small disparities of wealth and power between civil service employment grades led to significantly better health outcomes for the privileged. The more authority one has, the healthier one is.
Summarizing the social determinants of health model, Marmot and Wilkinson (1999) cite five findings from this research:
- “Differences in health between population groups are due to characteristics in society, not differences in health care.”
- “When people change social and cultural environments, their disease risks change.”
- “The health gradient is not a function of poverty alone” (meaning poor health for the poor and good health for the rest), rather it is a “…problem across the entire socioeconomic spectrum—as one moves down the social hierarchy, life expectancy gets shorter and mortality rates are higher.”
- The health gradient can change (and change quickly) with interventions.
- “The health gradient is not a matter of selection”—“…health does not determine social position, rather, social position determines health” (Marmot and Wilkinson, 1999)
Diverging from this quantitative approach, functionalism explains the social dynamics of health and illness in terms of social roles designated for those who are defined as ill compared to those who are defined as healthy. According to the functionalist perspective, health is vital to the stability of society, and therefore sickness is a form of deviance. Like other forms of deviance, it also has a function that determines the social role of the sick in society, regardless of the biological underpinnings of the illness. Talcott Parsons (1951) was the first to discuss this in terms of the sick role: patterns of expectations that define appropriate behaviour for the sick and for those who take care of them.
According to Parsons, the sick person has a specific social role with both rights and responsibilities. To start with, in the context of modern norms of individualism and individual responsibility, it is recognized that a person has not chosen to be sick and should not be treated as responsible for their condition. The sick person also has the right to be exempt from normal social roles; the person is not required to fulfill the obligation of a well person and can avoid normal responsibilities without censure. However, this exemption is temporary and relative to the severity of the illness. The exemption also requires medical legitimation by a physician; that is, a physician must certify that the illness is genuine.
The responsibility of the sick person is twofold: to try to get well and to seek technically competent help from a physician. If the sick person stays ill longer than is appropriate (malingers), they may be stigmatized.
Parsons argues that since the sick are unable to fulfill their normal societal roles, their sickness weakens society. Therefore, it is sometimes necessary for various forms of social control to bring the behaviour of a sick person back in line with normal expectations. In this model of health, doctors serve as gatekeepers, deciding who is healthy and who is sick — a relationship in which the doctor has all the power. The question of whether it is appropriate to allow doctors so much power over deciding who is sick typically falls outside the parameters of functionalist analysis.
Functionalists have traditionally assumed that medical diagnosis is universally accepted as legitimate, yet recent history reveals broad patterns of dissent from the authoritative positions of medical science. Similarly, there is the problem of people who become sick, but are unwilling to leave their normal positions for any number of reasons (personal/social obligations, financial need, or lack of medical insurance, for instance). Within the functional parameters of the sick role, the social structures that are responsible for providing health care can easily generate dysfunctional consequences that have disastrous impacts on individuals’ lived experience of illness.
Critical Sociology
Many explanations using the critical perspective suggest that issues with the health care system, as with most other social problems, are rooted in the power structures of capitalist society. A World Health Organization report studying the social determinants of health stated,
Poor and unequal living conditions are, in their turn, the consequence of deeper structural conditions that together fashion the way societies are organized – poor social policies and programmes, unfair economic arrangements, and bad politics. These ‘structural drivers’ operate within countries under the authority of governments, but also, increasingly over the last century and a half, between countries under the effects of globalization. This toxic combination of bad policies, economics, and politics is, in large measure, responsible for the fact that a majority of people in the world do not enjoy the good health that is biologically possible (W.H.O., 1988).
The reports’ authors noted that the crucial variable affecting health was not so much the overall wealth of a society, but of the equability of the distribution of wealth within societies.
Alongside the health disparities created by class inequalities, there are a number of health disparities created by racism, sexism, ageism, and heterosexism. The poor and socially excluded are more likely to experience illness caused by poor diet, physiological and psychological stress, living and working in unhealthy environments, and are less likely to challenge the system. In Canada for example, Indigenous people have been disproportionately marginalized from economic power, so they bear a great deal of the burden of poor health. In the critical approach, the empirical relationship between social determinants and health outcomes has to be understood in the broader context of historical formations of power and social inequality.
According to critical sociology, capitalism and the pursuit of profit also lead to the problematic commodification of health: the transformation of something not generally thought of as a commodity into something that can be bought and sold in a marketplace. In this view, corporations, private insurance companies, pharmaceutical companies and investors have a disproportionate influence over how the health care system is run and funded, which type of diseases are researched, whether cheaper generic versions of patented drugs can be sold, the delivery model and nature of the health care, and even how the physiology of the human body is understood.
One outcome of this is that corporate interests also influence the terms in which debates about public health care are discussed. Corporate think tanks like the Fraser Institute and the CD Howe Institute have long advocated free-market, profit-driven, American-style models rather than publicly funded models to deliver health care in Canada (Carroll and Shaw, 2001). The language with which they approach health care emphasizes “taxpayer rights,” critiques concerning the financial sustainability of public health care, and the role of unnamed “vested interests” in promoting an “outdated” 1960s-era system. Even though Canadians persistently state that public, universal health care is their central priority, corporate and neoliberal messaging on health care has become increasingly influential over the last three decades.

A different critical approach to health and illness focuses on analyzing the emergence of biopolitics in the 18th and 19th centuries (Foucault, 1980). As noted earlier in the chapter, biopolitics refers to the relationships of power that emerge when the task of fostering and administering the “life” of the population becomes central to the focus government (see also Chapter 17. Government and Politics). In a variety of different levels and sites in society — from implementing society-wide public health programs, sanitation procedures and population controls to various forms of disciplinary power exercised directly over the individual bodies of patients, soldiers, children, women, students, and prisoners — modern scientific knowledge on the functioning of the body establishes new power relations between experts (e.g., doctors, psychiatrists, psychologists, sociologists, social workers) and subjects. As a result, numerous forms of discipline and regulation emerge that seek to act upon the living body and the living population to maximize their potential for health, productivity, efficiency, and docility.
Modern biomedicine, for example, is a system of medical practice that defines health and illness in terms of the mechanics of the physical, biological systems of the human body. Its origin is in modern science’s division of mind and body as separate “substances.” This leads the individual to experience and inhabit their body and its problems in a certain way and to submit, voluntarily or involuntarily, to the expertise of doctors when bodily function deviates from biomedical norms. It is on the basis of doctors’ claim to biomedical knowledge about bodies that individuals submit to more or less mortifying exercises of power and discipline: from dieting and exercise regimes to pharmaceutical drug treatments to caesarean births to chemotherapy and gene therapy. See the discussion in Chapter 3. Culture of the “pop gene” for example.
It is interesting in this respect to note the various ways in which the knowledge and authority of doctors and the medical establishment are being challenged in contemporary society. People are increasingly researching and becoming more knowledgeable about their health concerns in a manner that permits them to engage with doctors and medical authorities on a more equal basis. They are also engaging with an expanding range of alternatives to conventional biomedicine: health practices and knowledge such as yoga, fitness training, dieting, acupuncture, traditional Chinese medicine, chi gong, naturopathy, homeopathy, chiropractic, and Indigenous healing practices.
This turn to a model of individualized care for the self — i.e., ways of acting independently upon the self to attain a certain mode of being such as “health” (Foucault, 1997) — has a number of competing implications, however. On the one hand, it enables practices of autonomy and self-formation freed from the power relations of the medical establishment. On the other hand, it can feed into intensified concerns and anxieties with the body that deepen rather than loosen submission to authorities and authoritative knowledge — dieting fads, esoteric knowledge and practices, and nontraditional healers, for example. As Zygmunt Bauman notes, when individuals take on the responsibility for knowledge about their own bodies and health in a pluralistic medical culture in which there are numerous competing and contradicting claims about treatment, the outcome for the individual can be paralyzing rather than liberating (Bauman, 2005).
Interpretive Sociology
According to theorists working in the interpretive perspective, health and illness are both socially constructed in crucial respects. As discussed in the beginning of the chapter, interpretive sociologists focus on the specific meanings and causes people attribute to illness. The medicalization of deviance is a prime example. As noted earlier, it refers to the social process that changes “bad” behaviour into “sick” behaviour, often to bring it under the social control of medical authorities. A related process is demedicalization, in which “sick” behaviour is normalized again by a social process of redefinition. Medicalization and demedicalization are examples that illustrate how understanding the variable meaning of illness requires an understanding of its social context. They affect who is considered to be a “patient,” who responds to the patient, how people respond to the patient, and how people view the personal responsibility of the patient (Conrad and Schneider, 1992).
Underlying the social construction of health and illness is an elemental distinction between what phenomenologists call Körper and Leib, or the physiological body and the lived body (Aho and Aho, 2008). Körper refers to the physical, externally observable body; what people are as physiological, neurological, and skeletal beings. Leib refers to the way in which the body is experienced from within, as well as how the world and physical existence are experienced sensually through the body. This applies to the distinction between a disease and an illness, although these terms are frequently used interchangeably in ordinary usage. A disease, therefore, refers to an organic based pathology which can in principle be measured through clinical or laboratory procedures. Illness, on the other hand, refers to the more unquantifiable subjective experience of ‘not feeling well.’
Phenomenologists argue that prior to the biomedical division of mind and body is the lived experience of the body. This distinction has implications for how interpretive sociologists study health and illness. Whereas science and biomedical research typically focus on the objective and measurable physiological characteristics of bodily life, people’s experiences of their bodies and bodily conditions can be at odds with these objective measures. For example, the same disease can be experienced as an illness in different ways or not experienced as an illness at all. A cancer can create debilitating discomfort and pain or not even be noticed until it is too late. One may be extremely ill with something like irritable bowel syndrome or chronic fatigue, but without any evident organic cause that would explain it in disease terms. Because these experiences of illness are typically unquantifiable, they require systematic interpretation to get a handle on.
As Aho and Aho (2008) elaborate:
If Körper is the abstract body-in-general, one object among others that is simply “there,” Leib is my body in particular, my life here and now, what I am as a volitional, sensing person…. however helpful the objective metrics of Körper may be—that is, in assessing caloric intake, blood pressure, lipid profiles, prostate specific antigens, and the like—they are inadequate when it comes to capturing the everyday experiences of appetite, stress, chest pain, or frequent nightly urination. The scientific measurement of the body, in other words, overlooks the actual lived experience of embodiment.
One key distinction that follows from this is the difference between being healthy or healed and being medically normal or cured. While these conditions often correspond, health refers to a much broader experience of wholeness, completeness, and balance, (implied in its linguistic association with the word “holiness”), than medical normality, which is more narrowly defined as the absence of disease. The World Health Organization’s (2014) definition of health, cited earlier in the chapter, is: “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” Recognizing this distinction enables sociology to expand the understanding of human health and illness beyond the framework of biomedicine to capture the patterns and nuances of people’s bodily experience.
Making Connections: Big Picture
Medicalization of Alcoholism and Demedicalization of Drapetomania
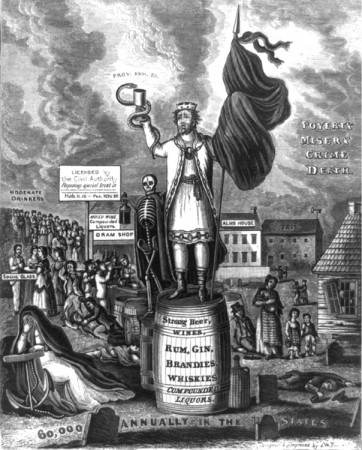
Another example of the medicalization of deviance is illustrated by the history of how Canadian society views alcohol and alcoholism. In general, medicalization is a social process that defines what behaviours and conditions are considered problematic in the first place, who is defined as a “patient,” who responds to the patient, how medical authorities and the general population respond to the patient, and how people view the personal responsibility of the patient (Conrad and Schneider, 1992). These processes of “problematization” apply to the evolution of how alcoholism has been defined historically in Canada.
During the 19th century, people who drank too much were considered bad, lazy people. They were called drunks, and it was common for them to be arrested or run out of a town. Drunks were not treated in a sympathetic way because, at that time, alcoholism was thought of as a moral failing; it was their own fault that they could not stop drinking.
By the late 19th century however, excessive drinking became regarded as a “disease of the will” — a defect in the will that undermined the ability to moderate or stop drinking (Valverde, 1997). This was a paradoxical illness that required the patient to use will power to actively engage in their own treatment, even though the nature of the disease was defined by a pathology of the will.
In the 20th century, people who drank too much were increasingly defined as alcoholics: people with a psychological dependence, physiological disease, or a genetic predisposition to addiction who were not responsible for their drinking. With alcohol use disorder defined as a psycho-physiological illness instead of a personal choice or matter of will power, dependence on alcohol came to be viewed with more compassion and understanding, although the paradox the “disease of the will” for recovery therapies for alcohol use disorder remained. Thus “badness” was transformed into “sickness” and a series of interventions, from group counseling (such as Alcoholics Anonymous) to medically supervised detox and withdrawal programs to pharmaceutical treatments, was devised to address it as an illness.
There are numerous examples of demedicalization in history as well. During the Civil War era in the United States, slaves who frequently ran away from their owners were diagnosed with a mental disorder called drapetomania. This has since been reinterpreted as a completely appropriate response to being enslaved. A more recent example is homosexuality, or same-gender attraction, which was labelled a mental disorder or a sexual orientation disturbance by the American Psychiatric Association until 1973. Similarly, in the 19th century, wealthy women were subject to frequent fainting spells, emotional shock, and attacks of hysteria, which disappeared once corsets and norms of female “delicacy” went out of fashion.
While interpretive sociology emphasizes the constructed nature of medical diagnosis, it is important to remember who most benefits when a behaviour becomes defined as illness. Pharmaceutical companies make billions treating illnesses such as fatigue, insomnia, and hyperactivity that may not actually be illnesses in need of treatment, but opportunities for companies to make more money. Moreover, the gradual medicalization and psychiatrization of the criminal justice system in the 19th and 20th centuries, as Michel Foucault (1979) has described, is an example of the establishment of a new center of authority and expertise. These extend the power of authorities and institutions to intervene into even more aspects of social life.
Media Attributions
- Figure 19.14 North Korea – Maternity hospital by Roman Harak, via Flickr, is used under a CC BY-SA 2.0 licence.
- Figure 19.15 King Alcohol and his Prime Minister, uploaded by , via Wikimedia Commons, is in the public domain. (Original uploader was JoeSmack ).

