11 Structure and Functions
Learning Objectives
At the end of this unit, you should be able to:
I. Define tissue and describe the importance of tissue level organization to an organism.
II. Describe the structure and function of epithelial, connective, muscle, and nervous tissue.
III. Explain the relationships between structure and function of tissues.
Learning Objectives and Guiding Questions
At the end of this unit, you should be able to complete all the following tasks, including answering the guiding questions associated with each task.
I. Define tissue and describe the importance of tissue level organization to an organism.
- What is a tissue?
- What is the main benefit to humans of having tissue level organization?
II. Describe the structure and function of epithelial, connective, muscle, and nervous tissue.
- Describe the general structure of each of the following:
- Epithelial tissue
- Connective tissue
- Muscle tissue
- Nervous tissue
- Describe the general function of each of the following:
- Epithelial tissue
- Connective tissue
- Muscle tissue
- Nervous tissue
- Compare and contrast the structure of the three types of connective tissue (proper, supportive connective tissue, and liquid connective tissue).
- Compare and contrast the structure of the three types of stratified epithelium (stratified squamous epithelium, stratified cuboidal epithelium, and stratified columnar epithelium).
III. Explain the relationships between structure and function of tissues.
- Use annotated diagrams to describe the structure and function of each of the seven main types of epithelial tissue (including pseudostratified columnar epithelium).
- Compare and contrast the structure and function of:
- Simple squamous epithelium and stratified squamous epithelium
- Simple squamous epithelium and simple columnar epithelium
- Simple squamous epithelium and simple cuboidal epithelium
- Simple cuboidal epithelium and simple columnar epithelium
- Simple cuboidal epithelium and stratified cuboidal epithelium
- Create a table stating:
- The matrix composition,
- The cellular types,
- The main function(s), and
- Specific examples
…of each of the following types of connective tissue:
-
- Fluid connective tissue
- Loose connective tissue
- Dense connective tissue
- Cartilage
- Bone
- Compare and contrast the three types of muscle tissue by discussing each of the following characteristics:
- The structure of each of the three types of muscle tissue
- How each type of muscle tissue is controlled (i.e., whether voluntary control is available or not)
- The function(s) of each of the three types of muscle tissue
- Name and describe both of the two main cell types in the nervous tissue. In your description, include:
- Their general cellular morphology (i.e., their shape)
- Their main function(s)
- What is the relationship between the structure and the function of the following tissues?
- Simple squamous epithelium
- Stratified squamous epithelium
- Fluid connective tissue
- Loose connective tissue
- Dense connective tissue
- Cartilage
- Bone
- Nervous tissue
The body contains at least 200 distinct cell types. These cells contain essentially the same internal structures, yet they vary enormously in shape and function. The different types of cells are not randomly distributed throughout the body; rather they occur in organized layers, a level of organization referred to as tissue.
Tissue: a higher level of organization
The term tissue is used to describe a group of cells found together in the body. The cells within a tissue share a common embryonic origin. Microscopic observation reveals that the cells in a tissue share morphological features and are arranged in an orderly pattern that achieves the tissue’s functions. From the evolutionary perspective, tissues appear in more complex organisms. For example, multicellular protists, ancient eukaryotes, do not have cells organized into tissues. Having tissue level organization increases the efficiency of the body as different shapes and internal structures are better suited to carry out different functions. Having different tissues for different functions allows for a greater speed of activity and a greater effectiveness in performing the various activities.
Although there are many types of cells in the human body, they are organized into four broad categories of tissues: epithelial, connective, muscle, and nervous. Each of these categories is characterized by specific functions that contribute to the overall health and maintenance of the body. A disruption of the structure is a sign of injury or disease. Such changes can be detected through histology, the microscopic study of tissue appearance, organization, and function.
The Four Types of Tissues
Epithelial tissue, also referred to as epithelium, refers to the sheets of cells that cover exterior surfaces of the body, lines internal cavities and passageways, and forms certain glands. Connective tissue, as its name implies, binds the cells and organs of the body together and functions in the protection, support, and integration of all parts of the body. Muscle tissue is excitable, responding to stimulation and contracting to provide movement, and occurs as three major types: skeletal (voluntary) muscle, smooth muscle, and cardiac muscle in the heart. Nervous tissue is also excitable, allowing the propagation of electrochemical signals in the form of nerve impulses that communicate between different regions of the body (Figure 1).
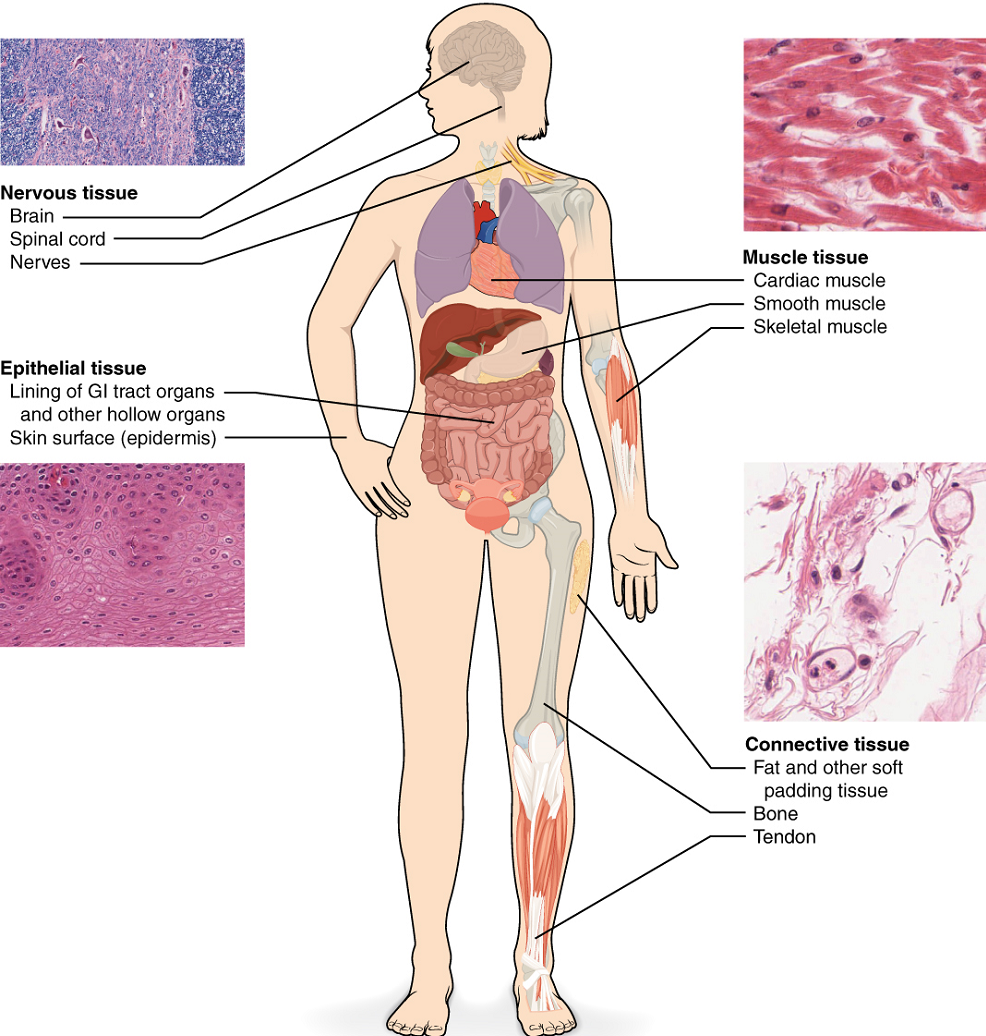
The next level of organization is the organ, where several types of tissues come together to form a working unit. Just as knowing the structure and function of cells helps you in your study of tissues, knowledge of tissues will help you understand how organs function. The epithelial and connective tissues are discussed in detail in this chapter. Muscle and nervous tissues will be discussed only briefly in this section.
Epithelial Tissue
Most epithelial tissues are essentially large sheets of cells covering all the surfaces of the body exposed to the outside world, and lining the outside of organs and the body cavities. Epithelium also forms much of the glandular tissue of the body. Skin is not the only area of the body exposed to the outside. Other areas include the airways, the digestive tract, as well as the urinary and reproductive systems, all of which are lined by an epithelium. Hollow organs and body cavities that do not connect to the exterior of the body, which includes, blood vessels and serous membranes, are lined by endothelium (plural = endothelia), which is a type of epithelium.
General Structure of Epithelial Tissue
All epithelia share some important structural and functional features. This tissue is highly cellular, with little or no extracellular material present between cells. The epithelial cells exhibit polarity with differences in structure and function between the exposed or apical facing surface of the cell and the basal surface close to the underlying body structures. Particular structures found in some epithelial cells are an adaptation to specific functions. Certain organelles are segregated to the basal sides, whereas other organelles and extensions, such as cilia, when present, are on the apical surface. The basal lamina, a mixture of glycoproteins and collagen, provides an attachment site for the epithelium, separating it from underlying connective tissue. The basal lamina attaches to a reticular lamina, which is secreted by the underlying connective tissue, forming a basement membrane that helps hold it all together.
Epithelial tissues are nearly completely avascular. For instance, no blood vessels cross the basement membrane to enter the tissue, and nutrients must come by diffusion or absorption from underlying tissues or the surface. Many epithelial tissues are capable of rapidly replacing damaged and dead cells. Sloughing off of damaged or dead cells is a characteristic of surface epithelium and allows our airways and digestive tracts to rapidly replace damaged cells with new cells.
General Functions of Epithelial Tissue
Epithelial tissues provide the body’s first line of protection from physical, chemical, and biological wear and tear. The cells of an epithelium act as gatekeepers of the body controlling permeability and allowing selective transfer of materials across a physical barrier. All substances that enter the body must cross an epithelium. Some epithelia often include structural features that allow the selective transport of molecules and ions across their cell membranes.
Many epithelial cells are capable of secretion and release mucous and specific chemical compounds onto their apical surfaces. The epithelium of the small intestine releases digestive enzymes, for example. Cells lining the respiratory tract secrete mucous that traps incoming microorganisms and particles. A glandular epithelium contains many secretory cells.
Classification of Epithelial Tissues
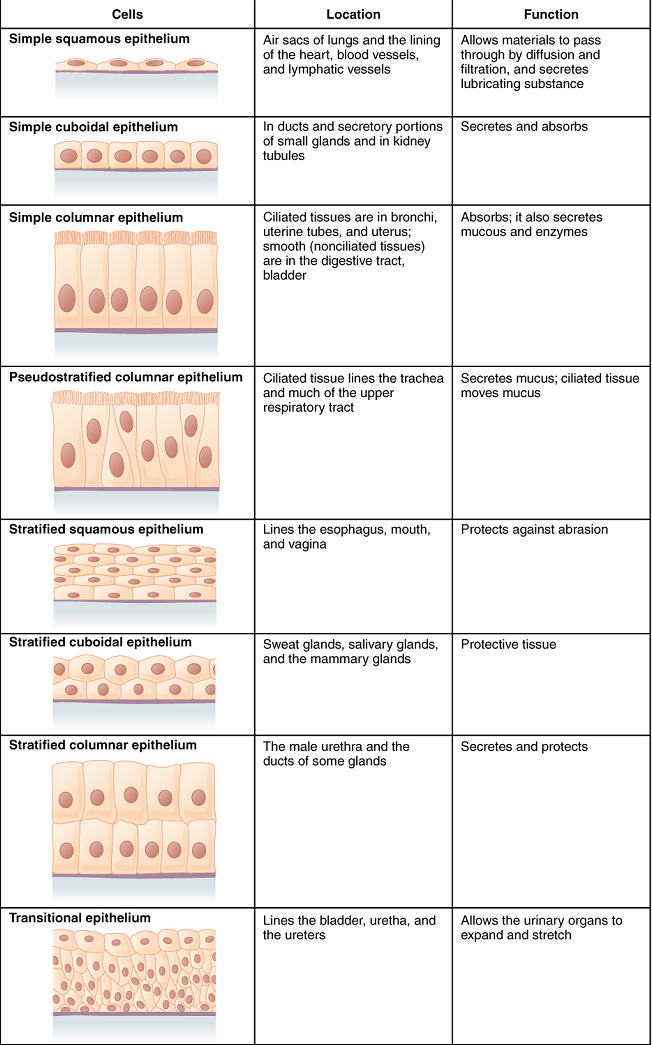
Epithelial tissues are classified according to the shape of the cells and number of the cell layers formed (Figure 2). Cell shapes can be squamous (flattened and thin), cuboidal (boxy, as wide as it is tall), or columnar (rectangular, taller than it is wide). Similarly, the number of cell layers in the tissue can be one—where every cell rests on the basal lamina—which is a simple epithelium, or more than one, which is a stratified epithelium and only the basal layer of cells rests on the basal lamina. Pseudostratified (pseudo- = “false”) describes tissue with a single layer of irregularly shaped cells that give the appearance of more than one layer. Transitional describes a form of specialized stratified epithelium in which the shape of the cells can vary.
Simple Epithelium: The shape of the cells in the single cell layer of simple epithelium reflects the functioning of those cells. The cells in simple squamous epithelium have the appearance of thin scales. Squamous cell nuclei tend to be flat, horizontal, and elliptical, mirroring the form of the cell. Simple squamous epithelium, because of the thinness of the cell, is present where rapid passage of chemical compounds is observed. The alveoli of lungs where gases diffuse, segments of kidney tubules, and the lining of capillaries are also made of simple squamous epithelial tissue.
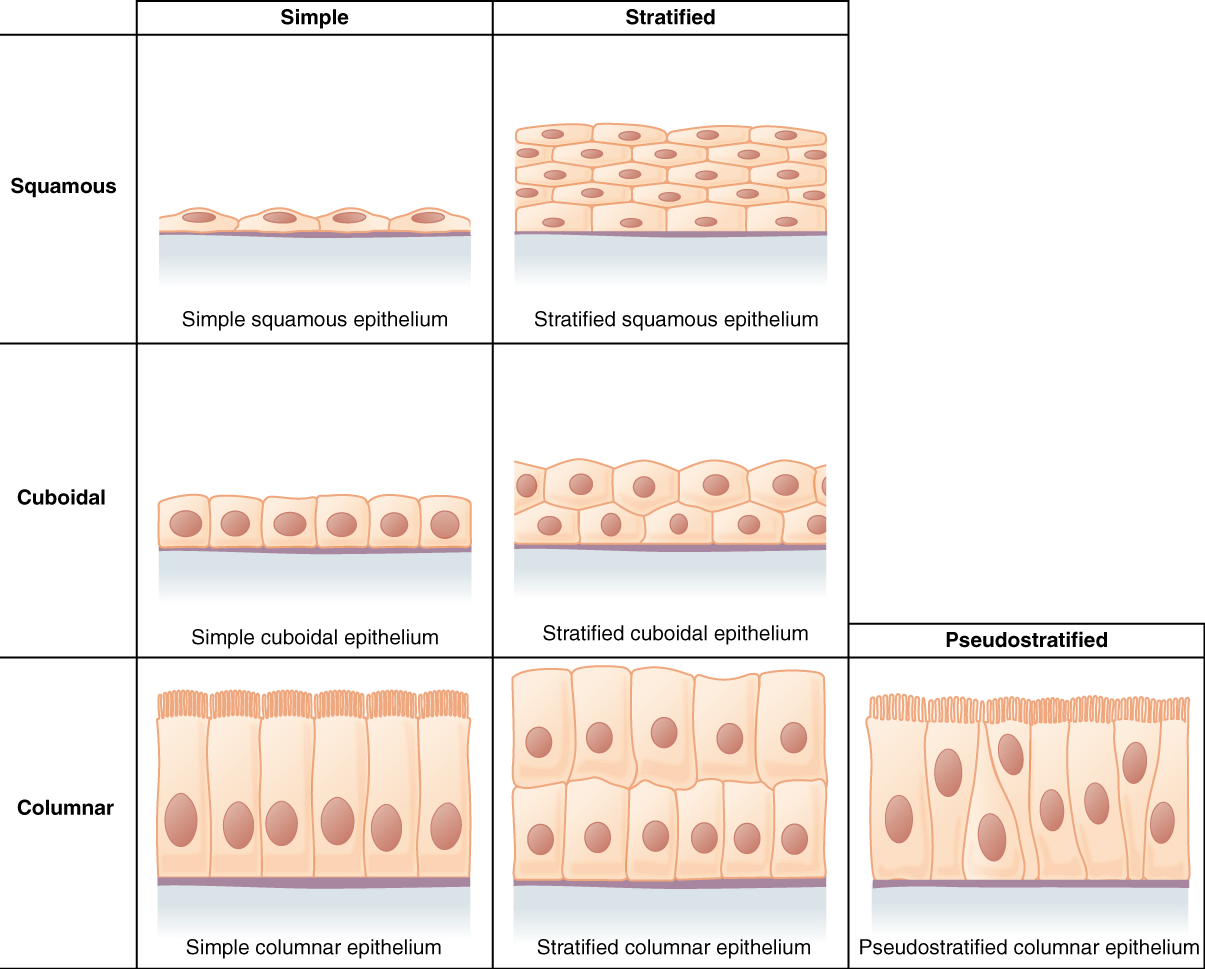
In simple cuboidal epithelium, the nucleus of the box-like cells appears round and is generally located near the center of the cell. These epithelia are active in the secretion and absorptions of molecules. Simple cuboidal epithelia are observed in the lining of the kidney tubules and in the ducts of glands (Figure 3).
In simple columnar epithelium, the nucleus of the tall column-like cells tends to be elongated and located in the basal end of the cells (Figure 3). Like the cuboidal epithelia, this epithelium is active in the absorption and secretion of molecules. Simple columnar epithelium forms the lining of some sections of the digestive system and parts of the female reproductive tract. Ciliated columnar epithelium is composed of simple columnar epithelial cells with cilia on their apical surfaces. These epithelial cells are found in the lining of the uterine tubes and parts of the respiratory system, where the beating of the cilia helps remove particulate matter.
Pseudostratified columnar epithelium is a type of epithelium that appears to be stratified but instead consists of a single layer of irregularly shaped and differently sized columnar cells. In pseudostratified epithelium, nuclei of neighbouring cells appear at different levels rather than clustered in the basal end (Figure 3). The arrangement gives the appearance of stratification; but in fact, all the cells are in contact with the basal lamina, although some do not reach the apical surface. Pseudostratified columnar epithelium is found in the respiratory tract, where some of these cells have cilia.
Stratified Epithelium: A stratified epithelium consists of several stacked layers of cells. This epithelium protects against physical and chemical wear and tear. The stratified epithelium is named by the shape of the most apical layer of cells, closest to the free space.
Stratified squamous epithelium is the most common type of stratified epithelium in the human body. The apical cells are squamous, whereas the basal layer contains either columnar or cuboidal cells. The top layer may be covered with dead cells filled with keratin. Mammalian skin is an example of this dry, keratinized, stratified squamous epithelium. The lining of the mouth cavity is an example of an nonkeratinized, stratified squamous epithelium. Stratified cuboidal epithelium and stratified columnar epithelium can also be found in certain glands and ducts, but are uncommon in the human body (Figure 3).
Watch this CrashCourse video to learn more about epithelial histology.
Connective tissue
General structure of connective tissue
As may be obvious from its name, one of the major functions of connective tissue is to connect tissues and organs. Unlike epithelial tissue, which is composed of cells closely packed with little or no extracellular space in between, connective tissue cells are dispersed in a matrix. The matrix usually includes a large amount of extracellular material produced by the connective tissue cells that are embedded within it. The matrix plays a major role in the functioning of this tissue. The major component of the matrix is a ground substance often crisscrossed by protein fibres. This ground substance is usually a fluid, but it can also be mineralized and solid, as in bones. Connective tissues come in a vast variety of forms, yet they typically have in common three characteristic components: cells, large amounts of amorphous ground substance, and protein fibres. The amount and structure of each component correlates with the function of the tissue, from the rigid ground substance in bones supporting the body to the inclusion of specialized cells; for example, a phagocytic cell that engulfs pathogens and also rids tissue of cellular debris.
Functions of Connective Tissues
Connective tissues perform many functions in the body, but most importantly, they support and connect other tissues; from the connective tissue sheath that surrounds muscle cells, to the tendons that attach muscles to bones, and to the skeleton that supports the positions of the body. Protection is another major function of connective tissue, in the form of fibrous capsules and bones that protect delicate organs and, of course, the skeletal system. Specialized cells in connective tissue defend the body from microorganisms that enter the body. Transport of fluid, nutrients, waste, and chemical messengers is ensured by specialized fluid connective tissues, such as blood and lymph. Adipose cells store surplus energy in the form of fat and contribute to the thermal insulation of the body.
Classification of Connective Tissue
The three broad categories of connective tissue are classified according to the characteristics of their ground substance and the types of fibres found within the matrix (Table 1). Connective tissue proper includes loose connective tissue and dense connective tissue. Both tissues have a variety of cell types and protein fibres suspended in a viscous ground substance. Dense connective tissue is reinforced by bundles of fibres that provide tensile strength, elasticity, and protection. In loose connective tissue, the fibres are loosely organized, leaving large spaces in between. Supportive connective tissue – bone and cartilage – provide structure and strength to the body and protect soft tissues. A few distinct cell types and densely packed fibres in a matrix characterize these tissues. In bone, the matrix is rigid and described as calcified because of the deposited calcium salts. In fluid connective tissue – lymph and blood – various specialized cells circulate in a watery fluid containing salts, nutrients, and dissolved proteins.
| Connective tissue proper | Supportive connective tissue | Fluid connective tissue |
|---|---|---|
Loose connective tissue
|
Cartilage
|
Blood |
Dense connective tissue
|
Bones
|
Lymph |
Connective Tissue Proper
Fibroblasts are present in all connective tissue proper (Figure 4). Fibroblasts are the most abundant cells in connective tissue proper. Fibrocytes, adipocytes, and mesenchymal cells are fixed cells, which means they remain within the connective tissue. Other cells move in and out of the connective tissue in response to chemical signals. Macrophages, mast cells, lymphocytes, plasma cells, and phagocytic cells are found in connective tissue proper but are actually part of the immune system protecting the body.
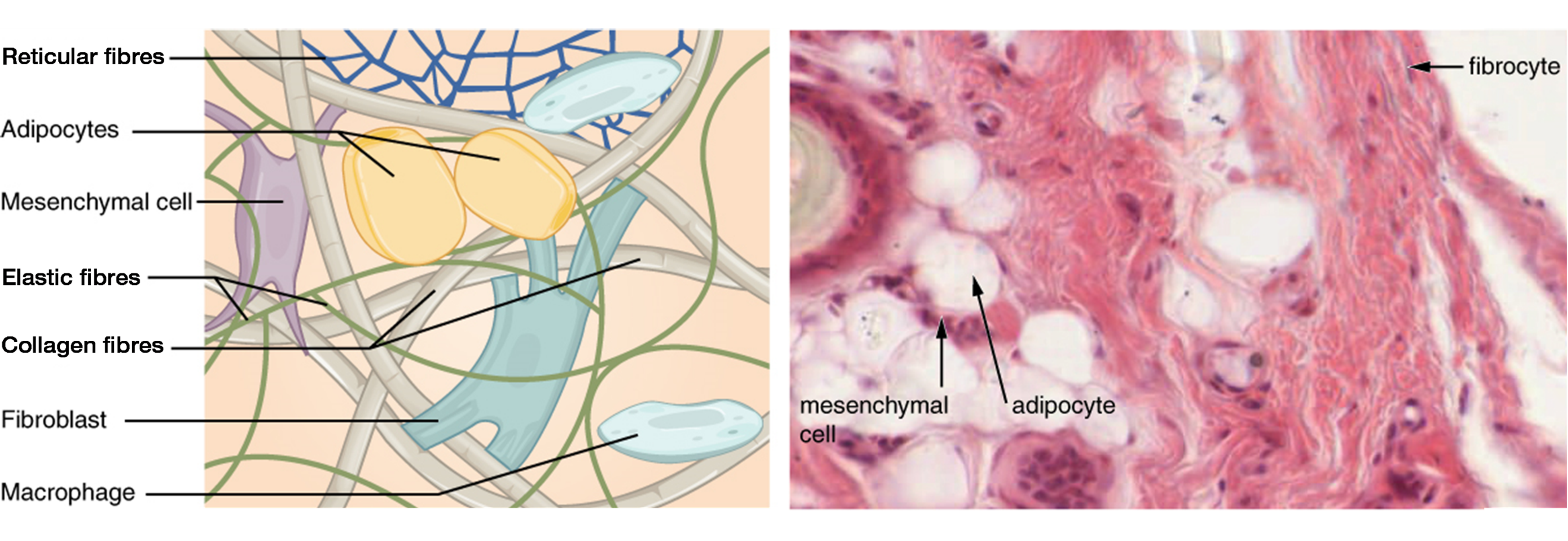
Adipocytes are cells that store lipids as droplets that fill most of the cytoplasm. The mesenchymal cell is a multipotent adult stem cell. These cells can differentiate into any type of connective tissue cells needed for repair and healing of damaged tissue. The macrophage is a large type of blood cell, which enters the connective tissue matrix from the blood vessels. The macrophage cells are an essential component of the immune system, which is the body’s defense against potential pathogens and degraded host cells. The mast cell found in connective tissue proper, when irritated or damaged, release histamine which causes vasodilation and increased blood flow at a site of injury or infection, along with itching, swelling, and redness you recognize as an allergic response.
Three main types of fibres are secreted by fibroblasts: collagen fibres, elastic fibres, and reticular fibres. Collagen fibres, while flexible, have great tensile strength, resist stretching, and give ligaments and tendons their characteristic resilience and strength. These fibres hold connective tissues together, even during the movement of the body. Elastic fibres after being stretched or compressed will return to its original shape. Elastic fibres are prominent in elastic tissues found in skin and the elastic ligaments of the vertebral column. Reticular fibres are narrow and are arrayed in a branching network. They are found throughout the body, but are most abundant in the reticular tissue of soft organs, such as liver and spleen, where they anchor and provide structural support to the parenchyma (the functional cells, blood vessels, and nerves of the organ). All of these fibre types are embedded in ground substance, a clear, viscous, colorless matrix made of polysaccharides and proteins, forming the extracellular matrix.
Loose Connective Tissue
Loose connective tissue is found between many organs where it acts both to absorb shock and bind tissues together. It allows water, salts, and various nutrients to diffuse through to adjacent or imbedded cells and tissues.
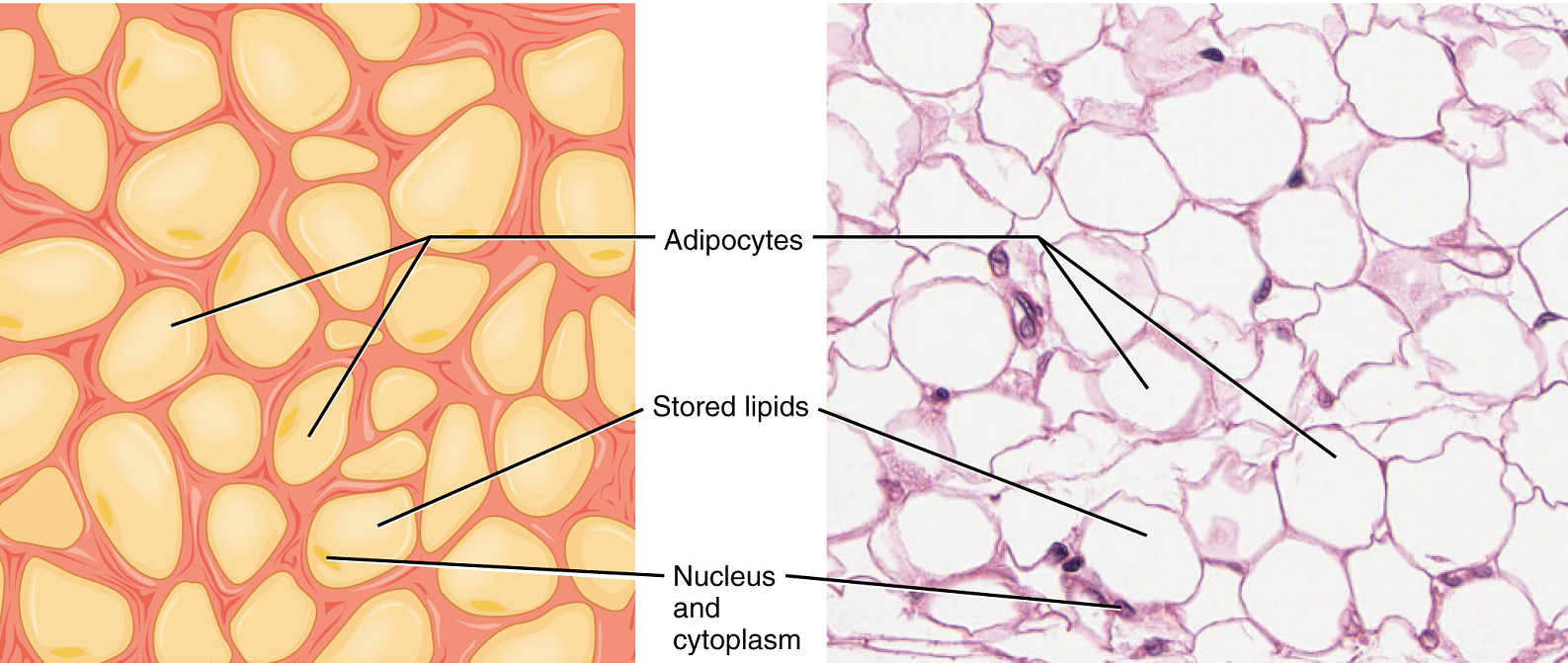
Adipose tissue consists mostly of fat storage cells, with little extracellular matrix (Figure 5). A large number of capillaries allow rapid storage and mobilization of lipid molecules. Fat contributes mostly to lipid storage and can serve as insulation from cold temperatures and mechanical injuries.
Areolar tissue shows little specialization. It contains all the cell types and fibres previously described and is distributed in a random, web-like fashion. It fills the spaces between muscle fibres, surrounds blood and lymph vessels, and supports organs in the abdominal cavity. Areolar tissue underlies most epithelia and represents the connective tissue component of epithelial membranes, which are described further in a later section.
Reticular tissue is a mesh-like, supportive framework for soft organs such as lymphatic tissue, the spleen, and the liver (Figure 6). Reticular cells produce the reticular fibres that form the network onto which other cells attach. It derives its name from the Latin reticulus, which means “little net.”

Dense Connective Tissue
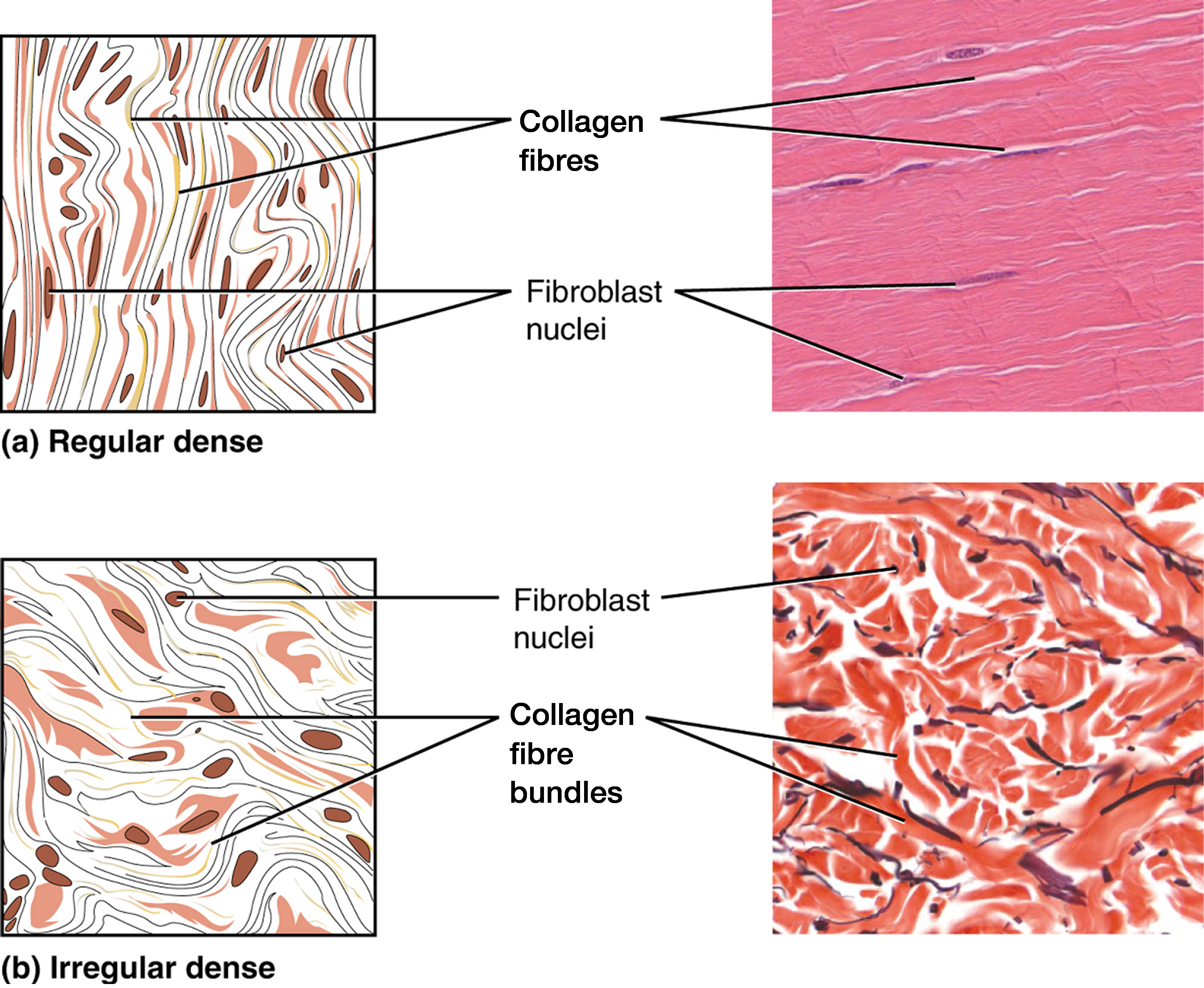
Dense connective tissue (also called fibrous connective tissue) contains more collagen fibres than does loose connective tissue. As a consequence, it displays greater resistance to stretching. There are two major categories of dense connective tissue: regular and irregular. Dense regular connective tissue fibres are parallel to each other, enhancing tensile strength and resistance to stretching in the direction of the fibre orientations. Ligaments and tendons are made of dense regular connective tissue, but in ligaments not all fibres are parallel. Dense regular elastic connective tissue contains elastin fibres in addition to collagen fibres, which allows the ligament to return to its original length after stretching. The ligaments in the vocal folds and between the vertebrae in the vertebral column are elastic.
In dense irregular connective tissue, the direction of fibres is random. This arrangement gives the tissue greater strength in all directions and less strength in one particular direction. In some tissues, fibres crisscross and form a mesh. In other tissues, stretching in several directions is achieved by alternating layers where fibres run in the same orientation in each layer, and it is the layers themselves that are stacked at an angle. The dermis of the skin is an example of dense irregular connective tissue rich in collagen fibres. Dense irregular elastic connective tissue give arterial walls the strength and the ability to regain original shape after stretching (Figure 7).
Supportive Connective Tissues
Two major forms of supportive connective tissue, cartilage and bone, allow the body to maintain its posture and protect internal organs.
Cartilage
The distinctive appearance of cartilage is due to polysaccharides, which bind with ground substance proteins to form the extracellular matrix. Embedded within the cartilage matrix are chondrocytes, or cartilage cells, and the space they occupy are called lacunae (singular = lacuna). A layer of dense irregular connective tissue, the perichondrium, encapsulates the cartilage. Cartilaginous tissue is avascular, thus all nutrients need to diffuse through the matrix to reach the chondrocytes. This is a factor contributing to the very slow healing of cartilaginous tissues.
The three main types of cartilage tissue are hyaline cartilage, fibrocartilage, and elastic cartilage (Figure 8). Hyaline cartilage, the most common type of cartilage in the body, contains short and dispersed collagen fibres in the matrix. Both strong and flexible, the hyaline cartilage is found in the rib cage and nose and covers bones where they meet to form moveable joints. It makes up a template of the embryonic skeleton before bone formation. A plate of hyaline cartilage at the ends of bone allows continued growth until adulthood. Fibrocartilage is tough because it has thick bundles of collagen fibres dispersed through its matrix. The knee and jaw joints and the intervertebral discs are examples of fibrocartilage. Elastic cartilage contains elastic fibres as well as collagen. This tissue gives rigid support as well as elasticity. Tug gently at your ear lobes, and notice that the lobes return to their initial shape. The external ear contains elastic cartilage.

Bone
Bone is the hardest connective tissue. It provides protection to internal organs and supports the body. Bone’s rigid extracellular matrix contains mostly collagen fibres embedded in a mineralized ground substance containing hydroxyapatite, a form of calcium phosphate. Both components of the matrix, organic and inorganic, contribute to the unusual properties of bone. Without collagen, bones would be brittle and shatter easily. Without mineral crystals, bones would flex and provide little support. Osteocytes, bone cells similar to chondrocytes, are located within lacunae. The histology of transverse tissue from long bone shows a typical arrangement of osteocytes in concentric circles around a central canal. Bone is a highly vascularized tissue. Unlike cartilage, bone tissue can recover from injuries in a relatively short time.
Cancellous bone (“trabecular bone” or “spongy bone”) looks like a sponge under the microscope and contains empty spaces between trabeculae, or arches of bone proper. It is lighter than compact bone and found in the interior of some bones and at the end of long bones. Compact bone is solid and has greater structural strength.
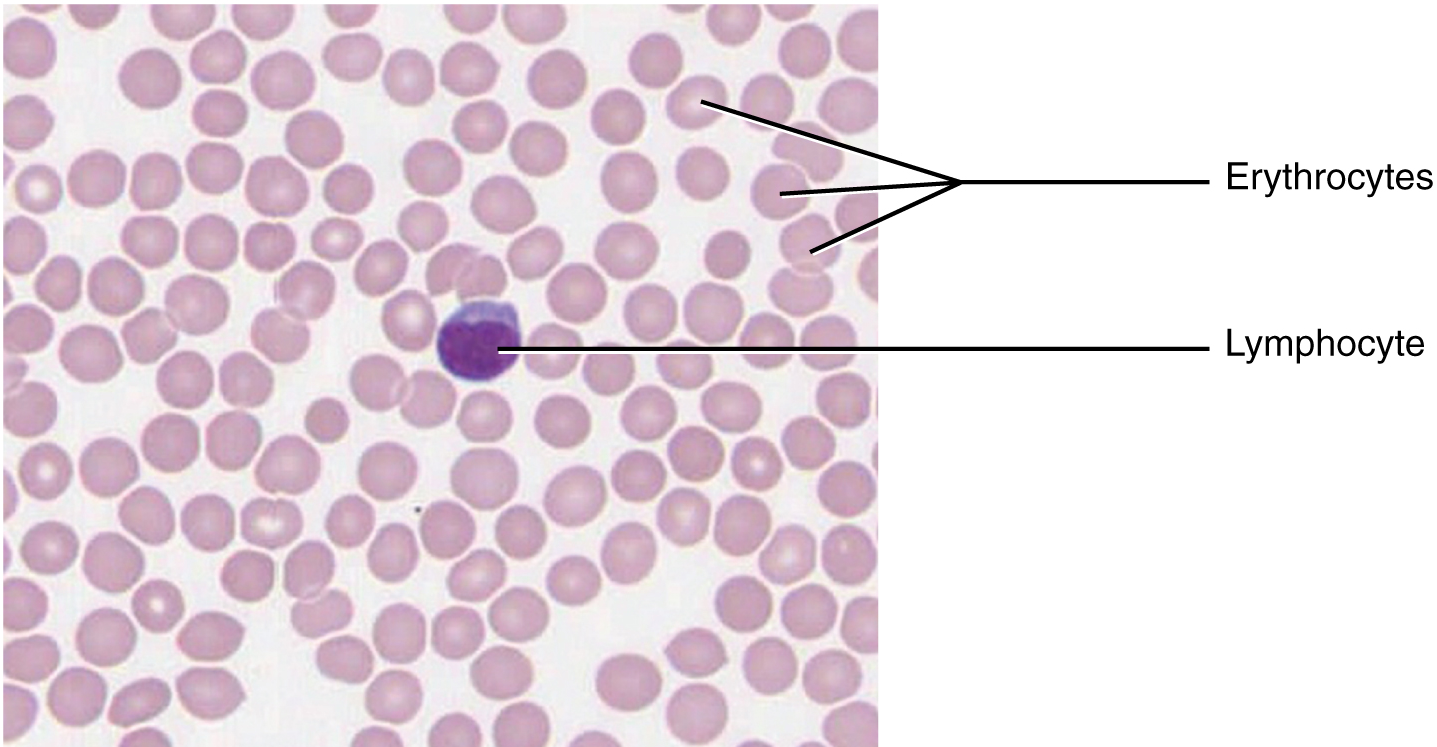
Fluid Connective Tissue
Blood and lymph are fluid connective tissues. Cells circulate in a liquid extracellular matrix. The formed elements circulating in blood are all derived from hematopoietic stem cells located in bone marrow (Figure 9). Erythrocytes, red blood cells, transport oxygen and some carbon dioxide. Leukocytes, white blood cells, are responsible for defending against potentially harmful microorganisms or molecules. Platelets are cell fragments involved in blood clotting.
Some white blood cells have the ability to cross the endothelial layer that lines blood vessels and enter adjacent tissues. Nutrients, salts, and wastes are dissolved in the liquid matrix and transported through the body.
Lymph contains a liquid matrix and white blood cells. Lymphatic capillaries are extremely permeable, allowing larger molecules and excess fluid from interstitial spaces to enter the lymphatic vessels. Lymph drains into blood vessels, delivering molecules to the blood that could not otherwise directly enter the bloodstream. In this way, specialized lymphatic capillaries transport absorbed fats away from the intestine and deliver these molecules to the blood.
Muscle Tissue
Muscle tissue is characterized by properties that allow movement. Muscle cells are excitable; they respond to a stimulus. They are contractile, meaning they can shorten and generate a pulling force. When attached between two movable objects, in other words, bones, contractions of the muscles cause the bones to move. Some muscle movement is voluntary, which means it is under conscious control. For example, a person decides to open a book and read a chapter on anatomy. Other movements are involuntary, meaning they are not under conscious control, such as the contraction of your pupil in bright light. Muscle tissue is classified into three types according to structure and function: skeletal, cardiac, and smooth (Table 2).
| Tissue | Histology | Function | Location |
|---|---|---|---|
| Skeletal | Long cylindrical fibre; striated; many peripherally-located nuclei | Voluntary movement; thermogenesis; organ protection | Attached to bones; found around entrance points to body (e.g. mouth, anus) |
| Cardiac | Short, branched fibres; striated; single central nucleus | Contracts to pump blood | Heart walls |
| Smooth | Short, spindle-shaped fibres; no evident striation; single nucleus | Involuntary movement; moves material through digestive tract and ducts; regulates blood flow in arteries | Walls of major organs and passageways |
Skeletal muscle
Skeletal muscle is attached to bones and its contraction makes possible locomotion, facial expressions, posture, and other voluntary movements of the body. Forty percent of your body mass is made up of skeletal muscle. Skeletal muscles generate heat as a byproduct of their contraction and thus participate in thermal homeostasis. Shivering is an involuntary contraction of skeletal muscles in response to perceived lower than normal body temperature.
The muscle cells, muscle fibres or myocytes, and their numbers remain relatively constant throughout life. Skeletal muscle tissue is arranged in bundles surrounded by connective tissue. Under the light microscope, muscle cells appear striated with many nuclei squeezed along the membranes (Figure 10a). The striation is due to the regular alternation of the contractile proteins actin and myosin, along with the structural proteins that couple the contractile proteins to connective tissues. The cells are multinucleated as a result of the fusion of the many myoblasts that fuse to form each long muscle fibre.
Cardiac muscle
Cardiac muscle forms the contractile walls of the heart. The cells of cardiac muscle, known as cardiomyocytes, also appear striated under the microscope. Unlike skeletal muscle fibres, cardiomyocytes are single cells typically with a single centrally located nucleus.
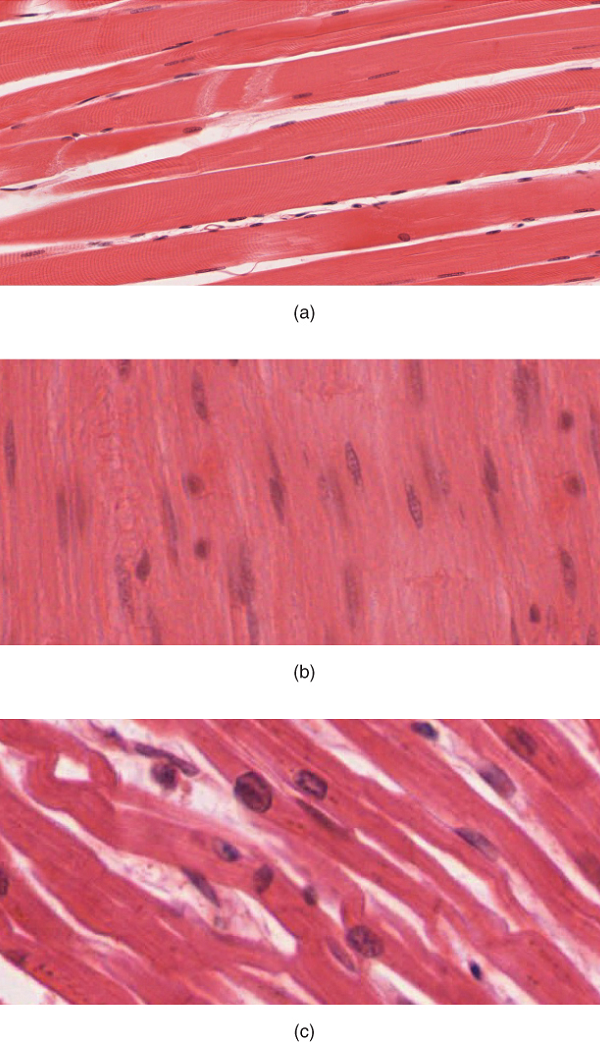
A principal characteristic of cardiomyocytes is that they contract on their own intrinsic rhythms without any external stimulation. Cardiomyocyte attach to one another with specialized cell junctions called intercalated discs. Attached cells form long, branching cardiac muscle fibres that are (Figure 10c), essentially, a mechanical and electrochemical syncytium allowing the cells to synchronize their actions. The cardiac muscle pumps blood through the body and is under involuntary control.
Smooth muscle tissue contraction is responsible for involuntary movements in the internal organs. It forms the contractile component of the digestive, urinary, and reproductive systems as well as the airways and arteries. Each cell is spindle shaped with a single nucleus and no visible striations (Figure 10b).
Nervous Tissue
Watch this CrashCourse video on tissues to learn more about muscle tissue.
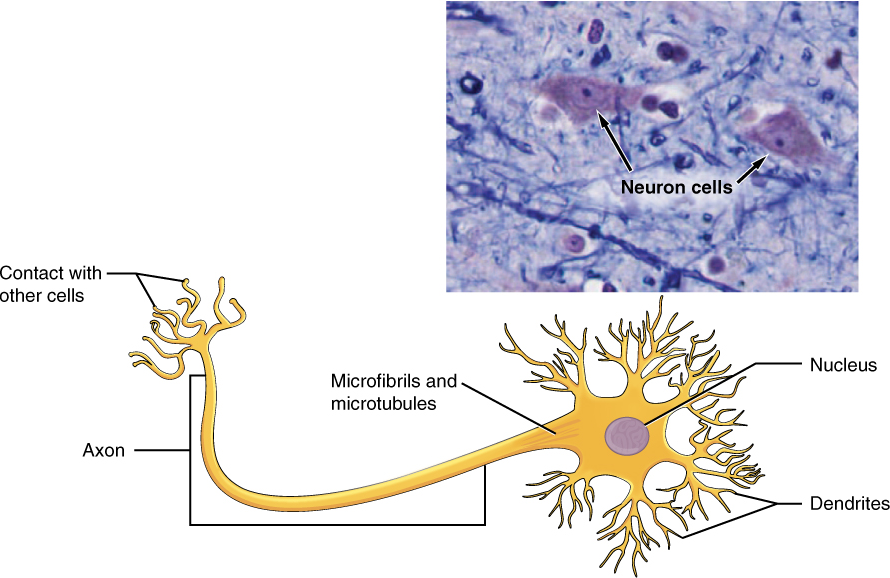
Nervous tissue is characterized as being excitable and capable of sending and receiving electrochemical signals that provide the body with information. Two main classes of cells make up nervous tissue: the neuron and neuroglia (Figure 11). Neurons propagate information via electrochemical impulses, called action potentials, which are biochemically linked to the release of chemical signals. Neuroglia play an essential role in supporting neurons and modulating their information propagation.
Neurons display distinctive morphology, well suited to their role as conducting cells, with three main parts. The cell body includes most of the cytoplasm, the organelles, and the nucleus. Dendrites branch off the cell body and appear as thin extensions. A long “tail,” the axon, extends from the neuron body and can be wrapped in an insulating layer known as myelin, which is formed by accessory cells. The synapse is the gap between nerve cells, or between a nerve cell and its target, for example, a muscle or a gland, across which the impulse is transmitted by chemical compounds known as neurotransmitters.
The second class of neural cells comprises the neuroglia or glial cells (Figure 12), which have been characterized as having a simple support role. The word “glia” comes from the Greek word for glue. Recent research is shedding light on the more complex role of neuroglia in the function of the brain and nervous system.
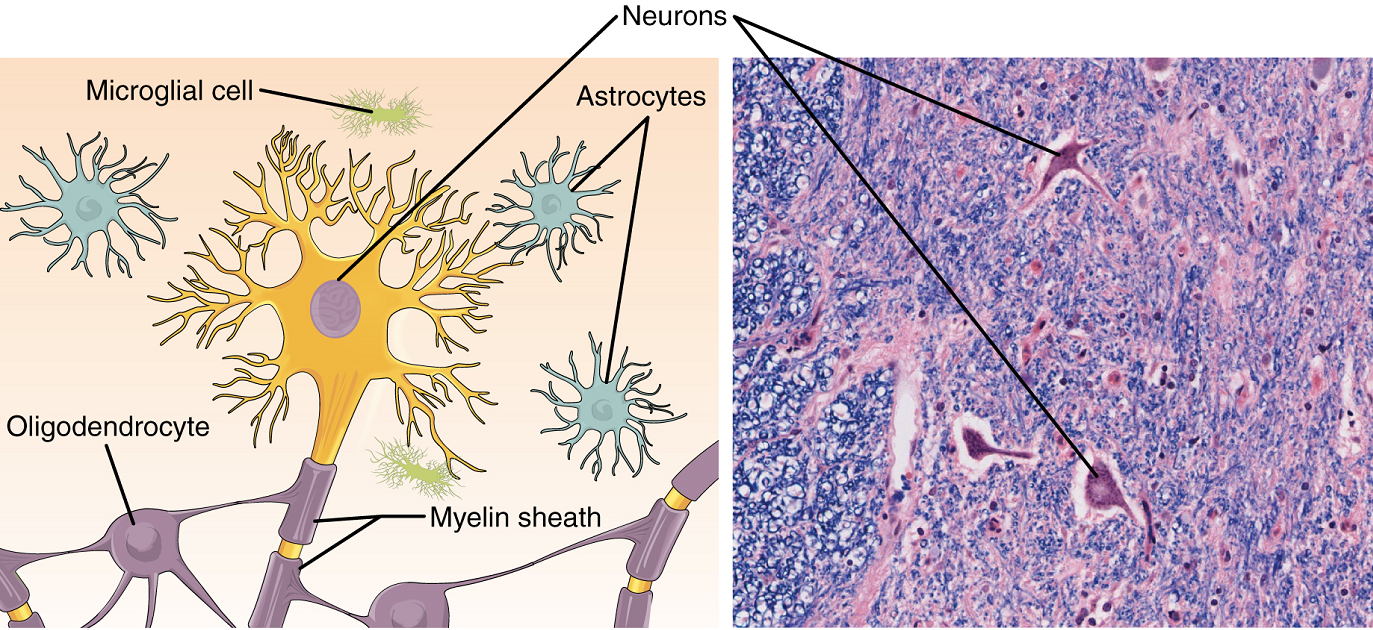
The presence of the nervous tissue throughout the body and its organization allow it to receive, integrate and provide information to the entire body. This ensures that appropriate responses can occur among all body systems within an intact organism, both under normal conditions as well as during times of stress.
Tissue: a higher level of organization
Epithelial tissue
Connective tissue
Muscle tissue
Nervous tissue
Attribution Note: Chapter remixed from Douglas College Human Anatomy & Physiology I by the Douglas College Biology Department.
Group of many similar cells (though sometimes composed of a few related types) that work together to perform a specific function.
Type of tissue that serves primarily as a covering or lining of body parts, protecting the body; it also functions in absorption, transport, and secretion.
Type of tissue that serves to hold in place, connect, and integrate the body’s organs and systems.
Microscopic study of tissue architecture, organization, and function.
(In physiology) under conscious control of the brain.
That part of a cell or tissue which, in general, faces an open space.
That part of a tissue close to underlying body structures.
Thin extracellular layer that lies underneath epithelial cells and separates them from other tissues.
Matrix containing collagen and elastin secreted by connective tissue; a component of the basement membrane.
In epithelial tissue, a thin layer of fibrous material that anchors the epithelial tissue to the underlying connective tissue; made up of the basal lamina and reticular lamina.
Lacking blood vessels.
Atom with an overall positive or negative charge. Many function as electrolytes.
Molecule (usually a protein) that catalyzes chemical reactions.
Tissue that consists of a single layer of flat scale-like cells; promotes diffusion and filtration across surface.
Tissue that consists of a single layer of cube-shaped cells; promotes secretion and absorption in ducts and tubules.
Tissue that consists of a single layer of column-like cells; promotes secretion and absorption in tissues and organs.
Small appendage on certain cells formed by microtubules and modified for movement of materials across the cellular surface (singular = cilium).
(Also, fallopian tube or oviduct) duct that facilitates transport of an ovulated oocyte to the uterus.
Tissue that consists of a single layer of irregularly shaped and sized cells that give the appearance of multiple layers; found in ducts of certain glands and the upper respiratory tract.
Tissue that consists of multiple layers of cells with the most apical being flat scale-like cells; protects surfaces from abrasion.
Type of structural protein that gives skin, hair, and nails its hard, water-resistant properties.
Tissue that consists of two or more layers of cube-shaped cells, found in some ducts.
Tissue that consists of two or more layers of column-like cells, contains glands and is found in some ducts.
(In connective tissue) extracellular material which is produced by the cells embedded in it, containing ground substance and fibres.
Fluid or semi-fluid portion of the matrix.
Cell process (a form of endocytosis) in which a cell engulfs and ingests another large particle or cell.
An infectious agent that causes disease, typically a bacterium, virus, fungus, or microscopic parasite.
Fluid contained within the lymphatic system, consisting of interstitial fluid, leukocytes (white blood cells), proteins (including antibodies) and fats.
Specialized areolar tissue rich in stored fat.
Connective tissue containing a viscous matrix, fibers, and cells.
Thick consistency between solid and liquid.
Most abundant cell type in connective tissue, secretes protein fibers and matrix into the extracellular space.
Mature, less active form of a fibroblast.
Lipid storage cells.
Embryonic tissue from which connective tissue cells derive.
Ameboid (irregular outline with peripheral projections) phagocyte found in several tissues throughout the body.
Cell found in the skin and the lining of body cells that contains cytoplasmic granules with vasoactive mediators such as histamine.
White blood cell characterized by a large nucleus and small rim of cytoplasm.
Differentiated B cell that is actively secreting antibody.
Describes the condition of being able to differentiate into different types of cells within a given cell lineage or small number of lineages, such as a red blood cell or white blood cell.
Cell that is oligo-, multi-, or pleuripotent that has the ability to produce additional stem cells rather than becoming further specialized.
(in immunology) referring to the organism in, or on, which a pathogen lives.
Vasoactive (active on blood vessels) mediator in granules of mast cells and is the primary cause of allergies and anaphylactic shock.
Opening up, or increasing interior (lumen) diameter of a blood vessel.
The most abundant of three protein fibres found in the extracellular matrix of connective tissues.
Fibrous protein within connective tissue that contains a high percentage of the protein elastin that allows the fibers to stretch and return to original size.
Fine fibrous protein, made of collagen subunits, which cross-link to form supporting “nets” within connective tissue.
Functional cells of a gland or organ, in contrast with the supportive or connective tissue of a gland or organ.
cartilage cells
(Plural= lacunae) small spaces in bone or cartilage tissue that cells occupy.
Layer of dense irregular connective tissue surrounding cartilage.
Most common type of cartilage, smooth and made of short collagen fibers embedded in a chondroitin sulfate ground substance.
Tough form of cartilage, made of thick bundles of collagen fibers embedded in chondroitin sulfate ground substance.
Type of cartilage, with elastin as the major protein, characterized by rigid support as well as elasticity.
A form of calcium phosphate mineral found in bones (also hydroxylapatite)
Primary cell in mature bone; responsible for maintaining the matrix.
Relating to circulation of blood.
(Also, cancellous bone) trabeculated osseous tissue that supports shifts in weight distribution.
(Also, hematopoiesis) production of the formed elements of blood.
Red blood cell.
White blood cell.
(Also, thrombocytes) one of the formed elements of blood that consists of cell fragments broken off from megakaryocytes.
Layer of smooth, simple squamous epithelium that lines the endocardium and blood vessels.
(In physiology) though under nervous control (usually from the brain), control is not conscious.
Usually attached to bone, under voluntary control, each cell is a fiber that is multinucleated and striated.
Heart muscle, under involuntary control, composed of striated cells that attach to form fibres, each cell contains a single nucleus, contracts autonomously.
Under involuntary control, moves internal organs, cells contain a single nucleus, are spindle-shaped, and do not appear striated; each cell is a fibre
Steady state of body systems that living organisms maintain.
Muscle cell (also muscle fibre).
Alignment of parallel actin and myosin filaments which form a banded pattern.
A multinucleate cell formed by the fusion of multiple cells or the division of nuclei.
Excitable neural cell that transfer nerve impulses.
Supportive neural cells.
Change in voltage of a cell membrane in response to a stimulus that results in transmission of an electrical signal; unique to neurons and muscle fibres.
Internal material between the cell membrane and nucleus of a cell, mainly consisting of a water-based fluid called cytosol, within which are all the other organelles and cellular solute and suspended materials.
Any of several different types of membrane-enclosed specialized structures in the cell that perform specific functions for the cell.
Cell’s central organelle; contains the cell’s DNA.
One of many branchlike processes that extends from the neuron cell body and functions as a contact for incoming signals (synapses) from other neurons or sensory cells.
Single process of the neuron that carries an electrical signal (action potential) away from the cell body toward a target cell.
Lipid-rich insulating substance surrounding the axons of many neurons, allowing for faster transmission of electrical signals.
Narrow junction across which a chemical signal passes from neuron to the next, initiating a new electrical signal in the target cell.
Chemical signal that is released from the synaptic end bulb of a neuron to cause a change in the target cell.

