18 Male Reproductive System
Learning Objectives
- Identify the anatomy of the male reproductive system
- Describe the main functions of the male reproductive system
- Spell the male reproductive system medical terms and use correct abbreviations
- Identify the medical specialities associated with the male reproductive system
- Explore common diseases, disorders, and procedures related to the male reproductive system
Male Reproductive System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Male Reproductive System.
Introduction to the Male Reproductive System
Gametes are the reproductive cells that combine to form a fetus. Organs called gonads produce the gametes, along with the hormones that regulate human reproduction. The male gametes are called sperm. Spermatogenesis occurs within the seminiferous tubules that make up most of the testis. The scrotum is a sac that holds the testes outside of the body cavity.
Watch this video:
Media 9.1. Reproductive System, Part 2 – Male Reproductive System: Crash Course A&P 41 [Online video]. Copyright 2015 by CrashCourse.
Male Reproductive Medical Terms
Anatomy (Structures) of the Male Reproductive System
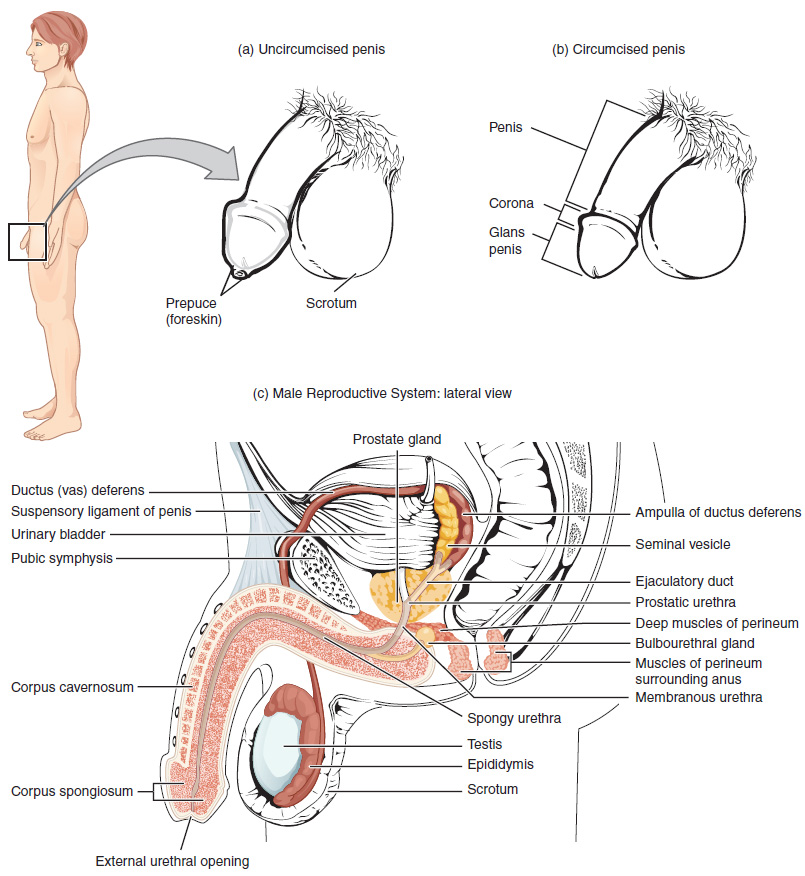
The structures of the male reproductive system include the testes, the epididymis, the penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the vas deferens. The spermatic cord is an enclosed sheath which includes the vas deferens, arteries, veins and nerves. The seminal vesicles and prostate gland add fluids to the sperm to create semen .
Physiology (Function) of the Male Reproductive System
Spermatogenesis
Spermatogenesis occurs in the seminiferous tubules that form the bulk of each testis. The process begins at puberty, after which time sperm are produced constantly throughout a man’s life. One production cycle takes approximately 64 days. One production cycle is considered from spermatogonia through to formed sperm. A new cycle starts approximately every 16 days, although this timing is not synchronous across the seminiferous tubules.
Sperm
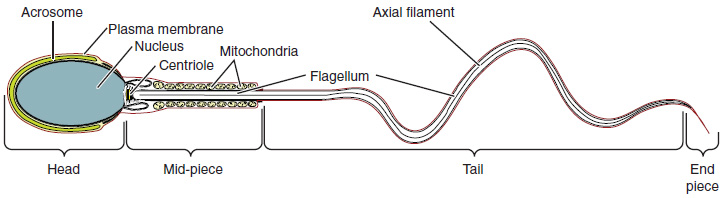
Sperm are smaller than most cells in the body; in fact, the volume of a sperm cell is 85,000 times less than that of the female gamete. Approximately 100 to 300 million sperm are produced each day, whereas women typically ovulate only one oocyte per month as is true for most cells in the body, the structure of sperm cells speaks to their function. Sperm have a distinctive head, mid-piece, and tail region (see Figure 9.2).
Sperm Transport
To fertilize an egg, sperm must be moved from the seminiferous tubules in the testes, through the epididymis, and—later during ejaculation—along the length of the penis and out into the female reproductive tract. It takes an average of 12 days for sperm to move through the coils of the epididymis, with the shortest recorded transit time in humans being one day.
Epididymis
Sperm enter the head of the epididymis and are moved by the contraction of smooth muscles lining the epididymal tubes. As the sperm mature they acquire the ability to move under their own power. Once inside the female reproductive tract, they will use this ability to move independently toward the unfertilized egg. The more mature sperm are then stored in the tail of the epididymis until ejaculation occurs.
Ducts
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the vas deferens (also called the ductus deferens). The vas deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord. From each epididymis, each vas deferens extends through the inguinal canal in the abdominal wall and continues to a region called the ampulla. The sperm is mixed with fluid from the paired seminal vesicles and moves into its associated ejaculatory duct. The ejaculatory ducts transport the seminal fluid to the prostate gland.
Prostate Gland
The prostate gland secretes an alkaline, milky fluid to the passing seminal fluid (referred to as semen) to first coagulate and then decoagulate the semen following ejaculation. The temporary thickening of semen helps retain it within the female reproductive tract and once decoagulated the sperm can pass farther into the female reproductive tract.
Bulbourethral Glands
Bulbourethral glands release a thick, salty fluid that lubricates the end of the urethra and vagina, and helps to clean urine residues from the penile urethra.
Concept Check
- Write or draw out the components of the pathway that sperms takes from beginning until the end.
- Consider fertility challenges that may be experienced if a large number of defective sperm are produced.
Anatomy Labeling Activity
Male Reproductive Terms not Easily Broken into Word Parts
Common Male Reproductive System Abbreviations
Diseases and Disorders
Erectile Dysfunction Disorder (EDD)
Erectile dysfunction (ED) is a condition in which a male has difficulty either initiating or maintaining an erection. The combined prevalence of minimal, moderate, and complete ED is approximately 40% in men at age 40 and reaches nearly 70% by 70 years of age. In addition to aging, ED is associated with diabetes, vascular disease, psychiatric disorders, prostate disorders, the use of some drugs such as certain antidepressants, and problems with the testes resulting in low testosterone concentrations. These physical and emotional conditions can lead to disruptions in the vasodilation pathway and result in an inability to achieve an erection (Betts, et al., 2013).
Cancer
Prostate Cancer
According to the Centers for Disease Control and Prevention (CDC), prostate cancer is the second most common cancer occurring in men. However, some forms of prostate cancer grow very slowly and may not require treatment. Aggressive forms of prostate cancer, in contrast, involve metastasis to organs like the lungs and brain. There is no link between Benign Prostatic Hyperplasia and prostate cancer, but the symptoms are similar. Prostate cancer is detected by medical history, a blood test, and a digital rectal exam that allows physicians to palpate the prostate and check for unusual masses. If a mass is detected, the cancer diagnosis is confirmed by biopsy of the cells (Betts, et al., 2013).
Testicular Cancer
Testicular cancer begins in the testicle or testis. It is most often found in men age 15 to 44 years, although it can be diagnosed at any age (Canadian Cancer Society, 2020). Testicular cancer is rare and treatable when diagnosed early. Common symptoms are a painless lump in the testicle, swelling, a heavy feeling in the scrotum or abdomen, amongst others. Sometimes, testicular cancer is found during infertility testing. An orchiectomy is the most common procedure for diagnosing and treating testicular cancer (Canadian Cancer Society, 2020). To learn more about testicular cancer, diagnosis and treatments please go to the Canadian Cancer Society’s web page on testicular cancer.
Sexually Transmitted Infections (STIs)
The terms for sexually transmitted infections (STI) and sexuality transmitted diseases (STD) are often used interchangeably. Sexuality transmitted disease (STD) implies the disease was acquired through sexual transmission. A disease is a disorder of structure or function in a human, which produces specific signs or symptoms. A disease must be managed, as with the case of human immunodeficiency virus (which can also be acquired through the transmission of other bodily fluids; thus not solely sexual transmission). The treatment may include antiretrovirals or anti-virals (Urology Care Foundation, 2019).
Chlamydia (CT)
Chlamydia is one of the most common sexually transmitted infections (STIs) caused by bacteria that infect the cervix, urethra and other reproductive organs. Chlamydia is easy to treat and can be cured. Many people with chlamydia do not have any symptoms and unknowingly pass the infection to their sexual partner(s). If symptoms develop, they usually appear two to six weeks after sexual contact with an infected person. Males may have penial discharge and itching around the urethra. The urethra is the opening in the penis. Males may also experience dysuria , polyuria , urethral pain and urethritis (Ontario Agency for Health Protection and Promotion , 2019; Region of Peel, 2007).
Chlamydia spreads through unprotected oral, anal or vaginal sex with an infected person. Chlamydia can be spread to the eyes via the hands with direct contact of infected fluids. Until a patient finishes their treatment, they continue to have the infection and can continue to pass it to others. Chlamydia is treated with antibiotic pills. If the patient has epididymitis, they may need to be hospitalized and be treated with intravenous (IV) antibiotics. All sexual partners within the past 60 days should be examined, treated, and informed that having no symptoms does not mean there is no infection (Ontario Agency for Health Protection and Promotion, 2019; Region of Peel, 2007).
Gonorrhea (Gonococcus) – (GC)
Gonorrhea is a sexually transmitted infection (STI) caused by bacteria that infects the cervix, urethra and other reproductive organs. Infections can also infect the throat and anus. Gonorrhea can be treated and cured. Many people infected with gonorrhea have no symptoms and can unknowingly pass the infection on to their sexual partner(s). If symptoms develop, they may appear two to seven days after sexual contact with an infected person. Symptoms vary depending on which part of the body is infected. Males may have yellowish-white discharge from the penis. They may also have dysuria , polyuria , testicular pain and testitis . Gonorrhea infection from oral sex may lead to sore throat and swollen glands. Gonorrhea infection from anal sex may cause itchiness and discharge from the anus. Gonorrhea is spread through unprotected oral, vaginal or anal sex with an infected person. Until the patient finishes their treatment, they continue to have the infection and can pass it to others (Ontario Agency for Health Protection and Promotion, 2019a; Region of Peel, 2007).
Gonorrhea is treated with oral antibiotics in combination with an intramuscular (IM) injection. It is important that one completes the treatment and abstain from unprotected sexual activity for at least seven days following treatment. If the patient develops epididymitis, the patient may need to go to a hospital and be treated with intravenous antibiotics.
All sexual partners within the past 60 days should be examined, treated and informed that having no symptoms does not mean there is no infection (Ontario Agency for Health Protection and Promotion, 2019a; Region of Peel, 2007).
Reportable Diseases
Both chlamydia and gonorrhea are reportable diseases to the Ministry of Health and Long Term Care. Therefore, the local health department will be calling the doctor’s office or patient to ensure correct treatment was received and sexual partners have been followed up with testing and treatment (Ontario Agency for Health Protection and Promotion, 2019a; Region of Peel, 2007). To learn more about STIs and STDs such as chlamydia and gonorrhea please go to the Public Health Ontario website.
Human Papillomavirus- HPV
HPV is another common sexually transmitted infection (STI). Both males and females can be infected with HPV. Around three quarters of sexually active individuals have been exposed to HPV during their lifetime. There are over 100 strains of HPV and some strains of HPV can cause visible genital warts. The warts are usually painless but may be itchy, uncomfortable and hard to treat. Some strains of HPV cause genital, anal, throat and cervical cancers. HPV spreads through sexual activity and skin-to-skin contact in the genital area with an infected person. Since some people are asymptomatic they don’t know they have the virus and consequently pass the virus to their sexual partners. Treatments are available for genital warts but there is no cure for HPV (York Region Health Connect, n.d.). To learn more about HPV symptoms, treatments, and prognosis visit the York Region Fact Sheet (PDF file) on HPV.
HPV Vaccine
A vaccine called Gardasil® 9 is available for 9 HPV strains. This vaccine assists the immune system in protecting the body against infections and diseases caused by HPV (York Region Health Connection, n.d.). To learn more about Gardasil® 9 treatments, please visit the Gardasil® 9 website.
Herpes Simplex Virus (HSV)
Genital herpes is a sexually transmitted infection (STI) that is caused by a virus called herpes simplex virus (HSV). There are two types of herpes simplex viruses:
- Type 1- oral herpes or cold sores (HSV-1)
- Type 2- genital herpes (HSV-2).
These viruses are very similar and either type can cause genital herpes or cold sores. Symptoms might include dysuria, enlarged glands, myalgia, arthralgia and fever. Once a patient is infected with HSV, the virus remains in their body even after the symptoms are gone and can cause recurring outbreaks. When the virus becomes active again, the symptoms return but are usually less painful and heal faster. Recurring outbreaks vary from person-to-person, however they can be triggered by emotional or physical stress, exposure to sunlight, hormonal changes, poor nutrition, sexual intercourse, lack of sleep or a low immune system.
Herpes is spread through direct contact with the sores or blisters of an infected person. Contact (and transfer of the virus) can occur from genitals-to-genitals, mouth-to-genitals or mouth-to-mouth. Herpes can also be passed to the anal area. Herpes spreads easily during sexual contact while symptoms are present, or just before an outbreak of symptoms. An infected person may spread herpes even when they have no symptoms; this is called asymptomatic shedding. One can spread the herpes virus to other parts of their body after touching the sores; autoinoculation. The fingers, eyes and other body areas can accidentally become infected in this way. Hand washing after touching sores and blisters is recommended to prevent spreading the virus.
There is no cure for herpes. Antiviral pills help to reduce symptoms and speed the healing of blisters or sores and are prescribed by a doctor. Treatment of symptoms may be managed with medication for pain, bath salts, cold compresses and urinating in water may help to relieve discomfort. Keep the infected area clean and dry, wear cotton underwear and loose clothing to reduce discomfort. All sexual partner(s) should be informed. The only way to reduce the risk of transmission of herpes is to avoid direct contact with the sores and to use condoms. Condoms will reduce but not eliminate risk as the virus can be present and shed from the skin in the genital area (Ontario Ministry of Health and Long-Term Care, 2015).
To learn more about the symptoms, complications, treatments and prognosis of HSV please visit the Ontario Ministry of Health and Long-Term Care’s Sexually Transmitted Diseases : Genital Herpes website or Public Health Ontario’s Testing Index.
STI Medical Abbreviations
Medical Terms in Context
Medical Specialties and Procedures related to the Male Reproductive System
Vasectomy
Watch the Animated Dissection of Anatomy for Medicine’s (A.D.A.M.) video to learn about a vasectomy. As described in this video, a vasectomy is a procedure in which a small section of the ductus (vas) deferens is removed from the scrotum. This cuts off the path taken by sperm through the ductus deferens. (as cited in Betts, et al., 2013).
No-Scalpel Vasectomy (NSV)
An alternative to a traditional vasectomy is the no-scalpel vasectomy (NSV). This is a minimally invasive procedure and an added benefit is that the recovery time is shorter. All vasectomies are completed by a urologist (Gentle Procedures Clinic, n.d.). To learn more about the NSV procedure, visit No-Scalpel Vasectomy Procedure Info by the Gentle Procedures Clinic in Toronto, Ontario.
Urology
Urology is a surgical sub specialty in which the surgeon has additional training in the treatments of diseases and disorders of the male and female urogenital systems (Canadian Medical Association, 2018). To learn more about urology and the training involved to become a urologist visit the Canadian Medical Association’s Urology Profile.
Male Reproductive Vocabulary
Arthralgia
Joint pain.
Bulbourethral glands
(Also, Cowper’s glands) glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation.
Corpus cavernosum
Either of two columns of erectile tissue in the penis that fill with blood during an erection.
Corpus spongiosum
(Plural = corpora cavernosa) column of erectile tissue in the penis that fills with blood during an erection and surrounds the penile urethra on the ventral portion of the penis.
Ductus deferens
(also, vas deferens) duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred as the vas deferens.
Dysuria
Painful urination.
Ejaculatory duct
Duct that connects the ampulla of the ductus deferens with the duct of the seminal vesicle at the prostatic urethra.
Epididymis
(plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation.
Epididymitis
Inflammation/swelling of the epididymis.
Gamete
Haploid reproductive cell that contributes genetic material to form an offspring.
Glans penis
Bulbous end of the penis that contains a large number of nerve endings.
Gonadotropin-releasing hormone (GnRH)
Hormone released by the hypothalamus that regulates the production of follicle-stimulating hormone and luteinizing hormone from the pituitary gland.
Gonads
Reproductive organs (testes in men and ovaries in women) that produce gametes and reproductive hormones.
Inguinal canal
Opening in abdominal wall that connects the testes to the abdominal cavity.
Leydig cells
Cells between the seminiferous tubules of the testes that produce testosterone, a type of interstitial cell.
Myalgia
Muscle pain.
Penis
Male organ of copulation.
Polyuria
Frequent urination.
Prepuce
(Also, foreskin) flap of skin that forms a collar around, and thus protects and lubricates, the glans penis; also referred as the foreskin.
Prostate gland
Doughnut-shaped gland at the base of the bladder surrounding the urethra and contributing fluid to semen during ejaculation.
Scrotum
External pouch of skin and muscle that houses the testes.
Semen
Ejaculatory fluid composed of sperm and secretions from the seminal vesicles, prostate, and bulbourethral glands.
Seminal vesicle
Gland that produces seminal fluid, which contributes to semen.
Seminiferous tubules
Tube structures within the testes where spermatogenesis occurs.
Sertoli cells
Cells that support germ cells through the process of spermatogenesis; a type of sustentacular cell.
Sperm
(Also, spermatozoon) male gamete.
Spermatic cord
Bundle of nerves and blood vessels that supplies the testes; contains ductus deferens.
Spermatid
Immature sperm cells produced by meiosis II of secondary spermatocytes.
Spermatocyte
Cell that results from the division of spermatogonium and undergoes meiosis I and meiosis II to form spermatids.
Spermatogenesis
Formation of new sperm, occurs in the seminiferous tubules of the testes.
Spermatogonia
Diploid precursor cells that become sperm (singular = spermatogonium).
Spermiogenesis
Transformation of spermatids to spermatozoa during spermatogenesis.
Testes
Male gonads (singular = testis).
Testitis
Inflammation of the testicles.
Urethritis
Inflammation of the urethra.
Test Yourself
References
Canadian Cancer Society. (2020). Symptoms of testicular cancer. https://www.cancer.ca/en/cancer-information/cancer-type/testicular/signs-and-symptoms/?region=on
Canadian Medical Association. (2018). Urology Profile. https://www.cma.ca/sites/default/files/2019-01/urology-e.pdf
CrashCourse. (2015, November 9). Reproductive system, part 2 – Male reproductive system: Crash course A&P 41. YouTube. https://youtu.be/-XQcnO4iX_U
Gentle Procedures Clinic. (n.d). No-Scalpel vasectomy procedure info. https://gentleprocedurestoronto.ca/vasectomy/no-scalpel-no-needle/
Ontario Agency for Health Protection and Promotion. (2019). Chlamydia. Public Health Ontario. https://www.publichealthontario.ca/en/diseases-and-conditions/infectious-diseases/sexually-transmitted-infections/chlamydia
Ontario Agency for Health Protection and Promotion. (2019a). Gonorrhea. Public Health Ontario. https://www.publichealthontario.ca/en/diseases-and-conditions/infectious-diseases/sexually-transmitted-infections/gonorrhea
Ontario Ministry of Health and Long-Term Care. (2015). Sexually transmitted diseases: Genital herpes (hur-peez). Publications. http://www.health.gov.on.ca/en/public/publications/std/herpes.aspx
Region of Peel. (2007). Chlamydia and Gonorrhea. https://www.peelregion.ca/health/talk-to-me/download/lesson-plans/lesson6-pdf/lesson6i.pdf
Urology Care Foundation. (2019). What are sexually transmitted infections (STIs) or diseases (STDs)?. https://www.urologyhealth.org/urologic-conditions/sexually-transmitted-infections#Acquired_Immune_Deficiency_Syndrome_(AIDS)
York Region Health Connection. (n.d.). Human Papillomavirus: https://www.york.ca/wps/wcm/connect/yorkpublic/b5158069-a667-4f43-bb25-e0449ba22caa/6052+Human+Papilloma+Virus+Fact+Sheet.pdf?MOD=AJPERES&CACHEID=b5158069-a667-4f43-bb25-e0449ba22caa
Image Descriptions
Figure 9.1 image description: This figure shows the different organs in the male reproductive system. The top panel shows the side view of a man and an uncircumcised and a circumcised penis. The bottom panel shows the lateral view of the male reproductive system and the major parts are labeled. [Return to Figure 9.1].
Figure 9.2 image description: This diagram shows the structure of sperm; the major parts are labeled (from left to right): head section (acrosome, plasma membrane, nucleaus), mid-piece (centriole, mitochondria, flagellum), tail (flagellum, axial filament), end piece (end piece). [Return to Figure 9.2].
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
haploid reproductive cells that contribute genetic material to form an offspring
reproductive organs (testes in men and ovaries in women) that produce gametes and reproductive hormones
Process of producing sperm
tube structures within the testes where spermatogenesis occurs
external pouch of skin and muscle that houses the testes
male gonads (singular = testis)
Blood vessels that transport blood away from the heart.
Blood vessels that carry blood back to the heart.
Collection of neurons; nerve cells
doughnut-shaped gland at the base of the bladder surrounding the urethra and contributing fluid to semen during ejaculation
male gamete (spermatozoon)
ejaculatory fluid composed of sperm and secretions from the seminal vesicles, prostate, and bulbourethral glands
diploid precursor cells that become sperm (singular = spermatogonium)
female gamete
(plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation
Pertaining to the epididymis
(also, ductus deferens) duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred as the vas deferens
(also, Cowper’s glands) glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation
Cancer spreads from one part of the body into another
male gonad (testes=plural)
Excision/removal of the testicle.
treatment that works against the virus replication
treatments that work effectively against a virus.
painful urination
frequent urination
inflammation of the urethra
swelling of the epididymis
Inflammation of the testicles
Antiobiotics are medications that stop bacterial infections.
pertaining to within the muscle
pertaining to without symptoms
pain in the muscles
painful joint(s)
self inoculation

