14 Providing Good Nutrition
Learning Objectives
By the end of this chapter, you should be able to:
- Describe the changes in nutritional needs as children mature (get older).
- Advocate for the support of breastfeeding mothers.
- Relate bottle-feeding practices.
- Discuss the transition to solid foods and self-feeding.
- Summarize feeding challenges for toddlers.
- Explain effective ways to respond to picky eating.
- Outline the importance of inclusive nutrition policies and practices.
- Identify how to support children with unique nutritional and feeding needs.
Introduction
To provide all children the appropriate nutrition, it is important to understand how nutritional needs and feeding practices change as children mature. Children with special needs may have different nutritional and feedings needs. Working with families and medical providers, programs can ensure that they meet each and every child’s needs. Early care and education programs can also support and empower families to provide the best nutrition to their children.
Feeding Infants
Requirements for macronutrients and micronutrients on a per-kilogram basis are higher during infancy than at any other stage in the human life cycle. See the average calorie needs for infants in Table 14.1. An infants’ resting metabolic rate is two times that of an adult. These needs are affected by the rapid cell division that occurs during growth, which requires energy and protein, along with the nutrients that are involved in DNA synthesis.[1]
| Table 14.1 – Average Calorie Needs for Infants [2] | |
| Sex/Age | Calories |
| Boys (0-6 months) | 472-645 calories |
| Girls (0-6 months) | 438-593 calories |
| Boys (6-12 months) | 645-844 calories |
| Girls (6-12 months) | 593-768 calories |
| Boys (1-2 years) | 844-1,050 calories |
| Girls (1-2 years) | 768-997 calories |
During this period, children are entirely dependent on their parents and other caregivers to meet these needs. For almost all infants six months or younger, breast milk is the best source to fulfill nutritional requirements. An infant may require feedings eight to twelve times a day or more in the beginning. After six months, infants can gradually begin to consume solid foods to help meet nutrient needs.
How often an infant wants to eat will also change over time due to growth spurts, which typically occur at about two weeks and six weeks of age, and again at about three months and six months of age.[3]
Breastfeeding
The dietary recommendations for infants are based on the nutritional content of human breast milk. Carbohydrates make up about 45 to 65 percent of the caloric content in breast milk. Protein makes up about 5 to 20 percent of the caloric content of breast milk. About 30 to 40 percent of the caloric content in breast milk is made up of fat. A diet in high unsaturated fat is necessary to encourage the development of neural pathways in the brain and other parts of the body.
Almost all of the nutrients that infants require can be met if they consume an adequate amount of breast milk. There are a few exceptions, though. Human milk is low in vitamin D, which is needed for calcium absorption and building bone, among other things. Breast milk is also low in vitamin K, which is required for blood clotting, and deficits could lead to bleeding or hemorrhagic disease. Infants are born with limited vitamin K, so supplementation may be needed initially and some states require a vitamin K injection after birth. Also, breast milk is not high in iron, but the iron in breast milk is well absorbed by infants. After four to six months, however, an infant needs an additional source of iron other than breast milk. Therefore, breastfed children often need to take a vitamin D supplement in the form of drops. [4]
Supporting Breastfeeding in Early Care and Education
Early care and education programs play an important role in supporting breastfeeding All staff members—despite their comfort or experience with breastfeeding—play an important role in breastfeeding promotion. They have an opportunity to share the facts about breastfeeding with families, and to help them decide what’s best for them and their babies.[5]

You can support breastfeeding mothers when you:
- Talk about why breastfeeding is so good for their infant.
- Tell them you want to care for breastfed infants and support breastfeeding mothers.
- Share other places in the community they can go to for help with breastfeeding.
- Share and discuss resources about breastfeeding.
- Try to time feedings to the mother’s schedule (being sure to respond to the infant’s needs and cues).
- Offer a place to nurse that is comfortable, quiet, and private.
- Communicate about their infant’s day.[6]
Feeding with Breastmilk in Early Care and Education Programs
Mothers may choose to have their breastfed infants fed in one of several ways when the infant is in child care including:
- Mother uses her breaks to come to the child care site at feeding times to nurse her infant;
- Child care provider gives the infant the breastmilk that the mother has expressed on a previous day.
Follow the feeding method that the mother chooses. Feeding advice such as the use of infant formula should come from the infant’s doctor or clinic.
Expressed breastmilk needs to be stored and handled safely to keep it from spoiling. Remind mothers to label, date, and chill or refrigerate their breastmilk right after they express it. Ask mothers to bring the milk in hard plastic bottles.
Ask mothers to bring in enough breastmilk to feed the infant each day. Be sure that each bottle or other container of breastmilk is labeled with the infant’s name and the date the milk was expressed. Bottles should have just the amount both you and the mother think the infant will take at each feeding. This amount will be about 2 to 4 ounces of breastmilk for the younger infant. As the infant gets older, the mother can put more breastmilk in each bottle. Keep breastmilk in the refrigerator or freezer until ready to use. Breastmilk that is not frozen, should be disposed of if not eaten within 72 hours.
Thaw frozen breastmilk by running the container under cool water. Do not set breastmilk out to thaw at room temperature. Do not thaw breastmilk by heating on the stove or in a microwave.[8] See below for instructions on how to bottle feed an infant.
Although breast milk is ideal for almost all infants, not all mothers will be able to breastfeed and some mothers should not breastfeed (including women with HIV, who are being treated for cancer, or who are taking drugs that are not safe while breastfeeding).
Formula Feeding
Infant formula provides a balance of nutrients. However, not all formulas are the same and there are important considerations that parents and caregivers must weigh. Standard formulas use cow’s milk as a base. They have 20 calories per fluid ounce, similar to breast milk, with vitamins and minerals added. Soy-based formulas are usually given to infants who develop diarrhea, constipation, vomiting, colic, or abdominal pain, or to infants with a cow’s milk protein allergy. Hypoallergenic protein hydrolysate formulas are usually given to infants who are allergic to cow’s milk and soy protein. This type of formula uses hydrolyzed protein, meaning that the protein is broken down into amino acids and small peptides, which makes it easier to digest.
Infant formula comes in three basic types:
- Powder that requires mixing with water. This is the least expensive type of formula.
- Concentrates, which are liquids that must be diluted with water. This type is slightly more expensive.
- Ready-to-use liquids that can be poured directly into bottles. This is the most expensive type of formula. However, it requires the least amount of preparation. Ready-to-use formulas are also convenient for traveling.
Most infants need about 2.5 ounces of formula per pound of body weight each day. Therefore, the average infant should consume about 24 fluid ounces of breastmilk or formula per day. When preparing formula, caregivers should carefully follow the safety guidelines, since an infant has an immature immune system. All equipment used in formula preparation should be sterilized. Prepared, unused formula should be refrigerated to prevent bacterial growth. Caregivers should make sure not to use contaminated water to mix formula in order to prevent foodborne illnesses. Follow the instructions for powdered and concentrated formula carefully—formula that is overly diluted would not provide adequate calories and protein, while overly concentrated formula provides too much protein and too little water which can impair kidney function.[9]
Feeding with Formula in Early Child Care and Education Programs
Early care and education programs provide commercially prepared formulas to infants, under the direction of the family. Bottles of formula should come prepared in bottles labeled with the infant’s name and the date. Unused mixed formula should not be stored for more than 24 hours.
Bottle Feeding (Both Expressed Breastmilk and Formula)
Always wash your hands before handling bottles or feeding the infant. Use only clean bottles, nipples, and cups. For infants that do not crawl, bottles and nipples should be sterilized. If you need to reuse them, sterilize by boiling in water for 5 minutes or by washing in a dishwasher.
Warm breastmilk and formula by placing the bottle in a pan of warm water or by holding it under warm running water for a few minutes. Do not warm breastmilk or formula on the stove or in a microwave. Microwave heating causes hot spots in the milk that can burn the infant’s mouth and throat. These hot spots may stay even if you shake the bottle. And heating also destroys most of the natural substances in breastmilk.

Double-check the labels on bottles before feeding to ensure the infant is getting the correct breastmilk or formula. Always hold the infant when bottle feeding. Try different positions for infants who do not want to take their bottles. Some infants are happier if you feed them in the usual cradle position. Others prefer a different position. Do not prop up a bottle to feed an infant or put an infant in a crib with a bottle. Bottle propping could cause the infant to choke, tooth decay, and ear infections.
Burp by placing the infant high over your shoulder or over your knee. You can also lean the infant forward in a sitting position supported by your hands. Pat or rub the infant’s back. This puts gentle pressure on the abdomen to push extra air from the stomach.[11]
Uneaten breastmilk or formula should be discarded after a feeding as bacteria from the infant’s mouth may have made it into the bottle.
When to Feed
In the early months, infants will need to be fed “on demand”—this means that they are able to feed whenever they are hungry or show hunger cues. Hunger cues are unique to each infant. An infant might:
- Have a specific hunger cry.
- Root or look around for food.
- Suck on their hand or fingers.
- Become irritable or restless.
- Repeat a unique behaviour to demonstrate hunger.
When adults respond to an infant’s hunger cues, the infant can also tell how much food they want and when they are full. This feeding practice supports healthy eating habits, growth, and development later in life.[12]
Pause to Reflect
Some families put infants on a schedule that dictates when they eat (and even sleep).
- Is this compatible with feeding on demand as described above?
- How might you discuss this with a family?
Introducing Solid Foods
Infants should be breastfed or formula-fed exclusively for the first six months of life according to the WHO. (The American Academy of Pediatrics recommends breast milk or bottle formula exclusively for at least the first four months, but ideally for six months.) Infants should not consume solid foods before six months because solids do not contain the right nutrient mix that infants need. Also, eating solids may mean drinking less breast milk or bottle formula. If that occurs, an infant may not consume the right quantities of various nutrients. If parents try to feed an infant who is too young or is not ready, their tongue will push the food out, which is called an extrusion reflex. After six months, the suck-swallow reflexes are not as strong, and infants can hold up their heads and move them around, both of which make eating solid foods more feasible.[13]
Knowing When an Infant is Ready for Solid Foods
Here are several ways you can tell that an infant is ready to eat solid foods:
- The infant’s birth weight has doubled.
- The infant can control their head and neck movements.
- The infant can sit up with some support.
- The infant can show you they are full by turning their head away or by not opening their mouth.
- The infant begins showing interest in food when others are eating.
Solid baby foods can be bought commercially or prepared from regular food using a food processor, blender, food mill, or grinder.[14] Baby food can be served at room temperature. If it is warmed, it must be stirred to distribute evenly.[15]
Portion the amount of food you intend to serve the baby (any uneaten food will need to be thrown away after a feeding and use small amounts on an infant-sized spoon. When beginning solid foods, timing is important. To keep mealtimes positive, choose a time when the infant is happy and when you have the patience and time to focus. Offer 1 to 2 teaspoons after a breastmilk or formula feeding. This can increase over time to 2 to 3 tablespoons.
It is normal for infants to refuse new foods. Sometimes it can take 10 to 12 times of offering a food before an infant will accept it. Infants know when they have had enough and may turn their head away. Don’t force them to keep eating.[16]
As families and caregivers introduce solids, they should feed the child only one new food at a time, to help identify allergic responses or food intolerances. An iron supplement is also recommended at this time.[17]
Foods to Avoid for Infants
- Never give honey to infants. It may contain bacteria that can cause botulism, a rare, but serious illness.
- Do not give infants cow’s milk until they are 1 year old. Before age 1, they have a difficult time digesting cow’s milk.
- Avoid foods with added salt or sugar.
- Do not give infants egg white until after they are 1 (egg yolks 3-4 per week are okay)[18]
Learning to Self-Feed
With the introduction of solid foods, young children begin to learn how to handle food and how to feed themselves. At six to seven months, infants can use their whole hand to pick up items (this is known as the palmer grasp). They can lift larger items, but picking up smaller pieces of food is difficult. At eight months, a child might be able to use a pincer grasp, which uses fingers to pick up objects.[19]
Serve food that is soft and mashed. Cut food into small pieces (cubes no larger than 1/4 inch) or thin slices that your baby can easily chew and swallow. Avoid high-risk choking foods such as small, slippery foods; dry foods that are hard to chew or sticky; and tough foods. [20]
Finger Foods
Here are some good food choices for self-feeding children:
- Soft cooked vegetables
- Washed and peeled fruits
- Graham crackers
- Melba toast
- Noodles
- Soft cooked vegetables
- Washed and peeled fruits
- Graham crackers
- Melba toast
- Noodles.
Here are foods to AVOID as they are a choking hazard:
- Apple chunks or slices
- Grapes
- Berries
- Raisins
- Dry flake cereals
- Hot dogs
- Sausages
- Peanut butter
- Popcorn
- Nuts

Figure 14.3 –This older infant has been served food on an unbreakable plate with a small utensil. [23] - Seeds
- Round candies
- Raw vegetables.[21]
To minimize choking, ensure that infants are seated while eating. If using a high chair, make sure to use the safety straps.[22]
After the age of one, children slowly begin to use utensils to handle their food. Unbreakable dishes and cups are essential, since very young children may play with them or throw them when they become bored with their food. [24]
Supporting Infant Nutrition
Nutrition during the first year of life is really important. While babies who are breastfed for at least 6 months are more likely to have a healthy weight as they grow up, mothers often report that breastfeeding is harder than they thought. And mothers may be more likely to stop breastfeeding if they feel unsupported and have nowhere to turn for help. And families that choose not to or cannot breastfeed have questions and need support to feed their infants in a healthy and safe way, too. Babies should be ready to start eating simple solids around 6 months. Babies who start eating solid foods too early are more likely to have weight problems as children and adults.[25]
Early care and education programs can support infant nutrition with the following practices:
- All food brought from home should be labeled with the child’s name and date.
- Part of the care plan that families share with their program and that is updated regularly, should be instructions for feeding. Families should determine how and what their infant is fed (as long as it’s in compliance with licensing).
- Support parents with materials on providing optimal nutrition for their infant (such as the tips just listed).
- Be supportive of mothers who are breastfeeding. For mothers who can come to nurse, provide a space conducive to that. Ensure the breastmilk that is brought to the program is properly labeled, stored, and prepared.
- For infants that are formula fed, ensure that formula is prepared according to the label (or doctor’s instructions).
- Hold all infants during bottle feedings. Not only does this keep them safe, but it is also valuable one-on-one time (caregiving routines are the heart of infant/toddler curriculum).
- Follow the cues of the infant you are feeding (when they are hungry and full).
- When feeding pureed baby food, use a small spoon and make sure you transfer food from a jar into a dish and throw away any uneaten food.
- Have appropriate seating available for infants that are beginning to self-feed (high chairs, booster seats, or enclosed small chairs at a low table)
- Provide unbreakable dishes to serve food to self-feeding infants.
Engaging Families in Supporting Their Infant’s Nutrition
Here are tips you can share with families
- If breastfeeding is harder than you thought it would be you are not alone!
- Lots of people say that breastfeeding just comes “naturally” but for many moms, it doesn’t.
- Going back to work and wanting to get back into a normal family routine can make it hard to stick with breastfeeding. Using a breast pump can help ensure your baby still gets the best nutrition.
- If you need support or help at any time while you are breastfeeding call 1-800-994-9662 (the National Breastfeeding Hotline) for free breastfeeding support.
- Don’t use pillows or other objects to hold a bottle for your baby. This makes it hard for her to spit out the bottle when she’s done – it can cause her to keep eating after she’s full.
- Make sure you take the bottle away if your baby falls asleep. If you let the baby keep the bottle in her mouth when he’s sleeping, formula can stay in her mouth and can damage his teeth or cause her to choke.
- Stick with ONLY breast milk or formula for feeding your baby until she is 6 months old. Unless your doctor tells you something different, adding cereal to a baby’s bottle adds extra calories to her diet that she doesn’t need. [26]
- Infants are usually ready to eat solid foods at about 6 months of age.
- If you introduce one new food at a time, you will be able to identify any foods that cause allergies in your baby.[27]
- Start solid feedings with iron-fortified baby cereal mixed with breast milk or formula. Mix it with enough milk so that the texture is very thin. Start by offering the cereal 2 times a day, in just a few spoonfuls.
- You can make the mixture thicker as your baby learns to control it in their mouth.
- You can also introduce iron-rich pureed meats, fruits, and vegetables. Try green peas, carrots, sweet potatoes, squash, applesauce, pears, bananas, and peaches.
- Some dietitians recommend introducing a few vegetables before fruits. The sweetness of fruit may make some vegetables less appealing.
- The amount your child eats will vary between 2 tablespoons (30 grams) and 2 cups (480 grams) of fruits and vegetables per day. How much your child eats depends on their size and how well they eat fruits and vegetables.[28]
Feeding Toddlers
Major physiological changes continue into the toddler years. Unlike in infancy, the limbs grow much faster than the trunk, which gives the body a more proportionate appearance. Their physical growth and motor development slow compared to the progress they made as infants. The toddler years pose interesting challenges for parents or other caregivers, as children learn how to eat on their own and begin to develop personal preferences. However, with the proper diet and guidance, toddlers can continue to grow and develop at a healthy rate.

The energy requirements for ages two to three are about 1,000 to 1,400 calories a day. In general, a toddler needs to consume about 40 calories for every inch of height. For example, a young child who measures 32 inches should take in an average of 1,300 calories a day. However, the recommended caloric intake varies with each child’s level of activity. Toddlers require small, frequent, nutritious snacks and meals to satisfy energy requirements. The amount of food a toddler needs from each food group depends on daily calorie needs.
Forty-five to 65% of their daily caloric intake should come from carbohydrates. Protein should make up 5 to 20% of their daily calories. And fat should make up 30 to 40% of their daily intake. Essential fatty acids are vital for the development of the eyes, along with nerve and other types of tissue. However, toddlers should not consume foods with high amounts of trans fats and saturated fats.
As a child grows bigger, the demands for micronutrients increase. These needs for vitamins and minerals can be met with a balanced diet, with a few exceptions. According to the American Academy of Pediatrics, toddlers and children of all ages need 600 international units of vitamin D per day. Vitamin D-fortified milk and cereals can help to meet this need. However, toddlers who do not get enough of this micronutrient should receive a supplement. Pediatricians may also prescribe a fluoride supplement for toddlers who live in areas with fluoride-poor water. Iron deficiency is also a major concern for children between the ages of two and three.[30]
Self-Feeding
As children grow older, they enjoy taking care of themselves, which includes self-feeding. During this phase, it is important to offer children foods that they can handle on their own and that helps them avoid choking and other hazards.

Examples include fresh fruits that have been sliced into pieces, orange or grapefruit sections, peas or potatoes that have been mashed for safety, a cup of yogurt, and whole-grain bread or bagels cut into pieces. Even with careful preparation and training, the learning process can be messy. As a result, parents and other caregivers can help children learn how to feed themselves by providing the following:
- Small utensils that fit a young child’s hand.
- Small cups that will not tip over easily.
- Plates with edges to prevent food from falling off.
- Small servings on a plate.
- Highchairs, booster seats, or small enclosed chairs to reach a low table.[31]
Feeding Challenges in the Toddler Years
During the toddler years, parents may face a number of problems related to food and nutrition. Possible obstacles include difficulty helping a young child overcome a fear of new foods, or fights over messy habits at the dinner table. Even in the face of problems and confrontations, parents and other caregivers must make sure their preschooler has nutritious choices at every meal. For example, even if a child stubbornly resists eating vegetables, parents should continue to provide them. Before long, the child may change their mind, and develop a taste for foods once abhorred. It is important to remember this is the time to establish or reinforce healthy habits.
Nutritionist Ellyn Satter states that feeding is a responsibility that is split between parent and child. According to Satter, parents are responsible for what their infants eat, while infants are responsible for how much they eat. In the toddler years and beyond, parents are responsible for what children eat, when they eat, and where they eat, while children are responsible for how much food they eat and whether they eat. Satter states that the role of a parent or a caregiver in feeding includes the following:
- Selecting and preparing food.
- Providing regular meals and snacks.
- Making mealtimes pleasant.
- Showing children what they must learn about mealtime behaviour.
- Avoiding letting children eat in between meal- or snack-times.
You are likely to notice a sharp drop in their child’s appetite. Children at this stage are often picky about what they want to eat. They may turn their heads away after eating just a few bites. Or, they may resist coming to the table at mealtimes. They also can be unpredictable about what they want to consume for specific meals or at particular times of the day. Although it may seem as if toddlers should increase their food intake to match their level of activity, there is a good reason for picky eating. A child’s growth rate slows after infancy, and toddlers ages two and three do not require as much food.[33]
Establishing healthy meal routines is an important step in healthy toddler development. Ideally, mealtimes should take place at regular times, at a table with limited distraction, and children should be encouraged to feed themselves with adult support as needed. [34] Best practices in early care and education include creating positive meal and snack times that are served family-style with adult modeling eating balanced nutrition.
Engaging Families in Supporting Their Toddler’s Nutrition
Here are tips you can share with families:
- Serving sizes for toddlers are much smaller than serving sizes for adults.
- A typical serving size for a toddler drink is 4-6 ounces. Water and milk are the best choices for toddlers.
- Your toddler (and you too!) needs food from all five of the food groups—grains, protein, vegetables, fruit, and dairy. Try offering a variety of foods from these groups at meals and snacks.
- Your toddler may eat more some days and less on others. Don’t worry, this is normal! Keep offering regularly scheduled meals and snacks.
- Allow your toddler to tell you when she is full. This teaches them to listen to their body for signs of hunger or fullness.
- Try using child-size plates, bowls, and utensils for “right-size” portions for your toddler. Using child-size utensils also makes it easier for your toddler to eat.
- Encourage toddlers to drink from cups and avoid the use of bottles or sippy cups.
- Limit distractions during meal and snack times to allow your toddler to enjoy the food. Turn off the TV and sit at a table.
- Toddlers get hungry between meals. Snack time is a great chance to feed your toddler healthy foods (like fruits and veggies).
- Remember to have a start and end time for snack time. Toddlers should not be snacking (or grazing) all day.[35]
Feeding Preschoolers
Children’s attitudes and opinions about food deepen. They not only begin taking their cues about food preferences from family members, but also from peers and the larger culture.

This time in a child’s life provides an opportunity for families and other caregivers to reinforce good eating habits and to introduce new foods into the diet while remaining mindful of a child’s preferences. Adults should also serve as role models for their children, who will often mimic their behaviour and eating habits.[36] MyPlate also provides a guide daily for calories based on sex and activity-level for preschool-aged children (although children’s needs may differ from the average and appetites can vary from day to day).
Table 14.1 – Average Calorie Needs for Preschoolers [38]
In early childhood, children should still get 45-65% of their daily calories from carbohydrates. Carbohydrates high in fiber should make up the bulk of intake. Their intake of protein increases to 10–30% of their daily calories to support muscle growth and development. High levels of essential fatty acids are needed to support growth (although not as high as in infancy and the toddler years). As a result, the daily recommendation for fat is 25–35% of their daily calories. And they should get 17–25 grams of fiber per day.
Their micronutrient needs should be met with foods first. Families and caregivers should select a variety of foods from each food group to ensure that nutritional requirements are met. Because children grow rapidly, they require foods that are high in iron, such as lean meats, legumes, fish, poultry, and iron-enriched cereals. Adequate fluoride is crucial to support strong teeth. One of the most important micronutrient requirements during childhood is adequate calcium and vitamin D intake. Both are needed to build dense bones and a strong skeleton. Children who do not consume adequate vitamin D should be given a supplement of 10 micrograms (400 international units) per day.[39]
Feeding Challenges in the Preschool Years
Picky eating is typical for many preschoolers. It’s simply another step in the process of growing up and becoming independent. As long as a preschooler is healthy, growing normally, and has plenty of energy, they are most likely getting the nutrients they need.
Typical Picky Eating Behaviors
Many children will show one or more of the following behaviours during the preschool years. In most cases, these will go away with time.
- Refusal of a food based on a certain colour or texture. For example, they could refuse foods that are red or green, contain seeds, or are squishy.
- Only eating a certain type of food. A preschooler may choose 1 or 2 foods they like and refuse to eat anything else.
- “Wasting” of time at the table and seeming interested in doing anything but eating.
- Unwillingness to try new foods. It is normal for a preschooler to prefer familiar foods and be afraid to try new things.[40]
Helping Families Cope with Picky Eating
Picky eating is temporary. If adults don’t make it a big deal, it will usually end before school age. The following tips are tips to help deal with picky eating behaviour positively.
- Let your kids be “produce pickers.” Let them pick out fruits and veggies at the store.
- Have your child help you prepare meals. Children learn about food and get excited about tasting food when they help make meals. Let them add ingredients, scrub veggies, or help stir.
- Offer choices. Rather than ask, “Do you want broccoli for dinner?” ask “Which would you like for dinner, broccoli or cauliflower?”
- Enjoy each other while eating family meals together. Talk about fun and happy things. If meals are times for family arguments, your child may learn unhealthy attitudes toward food.
- Offer the same foods for the whole family. Serve the same meal to adults and kids. Let them see you enjoy healthy foods. Talk about the colours, shapes, and textures on the plate.[41]
- Make food fun.
- Cut food into fun and easy shapes with cookie cutters.
- Encourage your child to invent and help prepare new snacks.
- Name a food your child helps create.[42]
- Focus on the meal and each other. Your child learns by watching you. Children are likely to copy your table manners, your likes and dislikes, and your willingness to try new foods.
- Offer a variety of healthy foods. Let your child choose how much to eat. Children are more likely to enjoy a food when eating it is their own choice.
- Let your children serve themselves. Teach your children to take small amounts at first. Let them know they can get more if they are still hungry.[43]
Trying New Foods
It is normal for children to reject foods they have never tried before. Here are some tips to get preschoolers to try new foods:
- Small portions, big benefits. Let children try small portions of new foods that you enjoy. Give them a small taste at first and be patient with them.
- Offer only one new food at a time and ideally with a favoured food. Offering many new foods all at once could be too much for children.
- Be a good role model. Try new foods yourself. Describe their taste, texture, and smell to the children.
- Offer new foods first when children are most hungry.
- Offer new foods many times. It may take up to a dozen tries for a child to accept a new food.[44]
Pause to Reflect
Think back to your childhood.
- Were you a picky eater or more adventurous?
- Why do you think that it was?
- How did your caregivers respond to your eating preferences?
- Do you have similar preferences now or have you expanded your tastes/preferences?
Feeding School-Aged Children
While calorie needs go up as children get older, until around age 9 (or the beginning of puberty), nutritional needs for school-aged children are very similar to preschoolers. Once puberty begins, there is a period of rapid growth as girls grow 2-8 inches and boys grow 4-12 inches.
Table 14.2 – Average Calorie Needs for School-Aged Children [45]
School-aged children should still get 45-65% of their daily calories from carbohydrates. Carbohydrates high in fiber should make up the bulk of that. Their intake of protein remains at 10–30% of their daily calories to support muscle growth and development. And the daily recommendation for fat also remains at 25–35% of their daily calories.
A few micronutrients take on added importance, especially at the beginning of puberty. These include vitamins, D, K, and B12, calcium, and iron. Whenever possible these additional micronutrient needs should be met with dietary choices and not supplements (with the exception of iron).[46]
School Meals
School-aged children can often eat both breakfast and lunch at school, which can save families time and provide children with nutritious food.
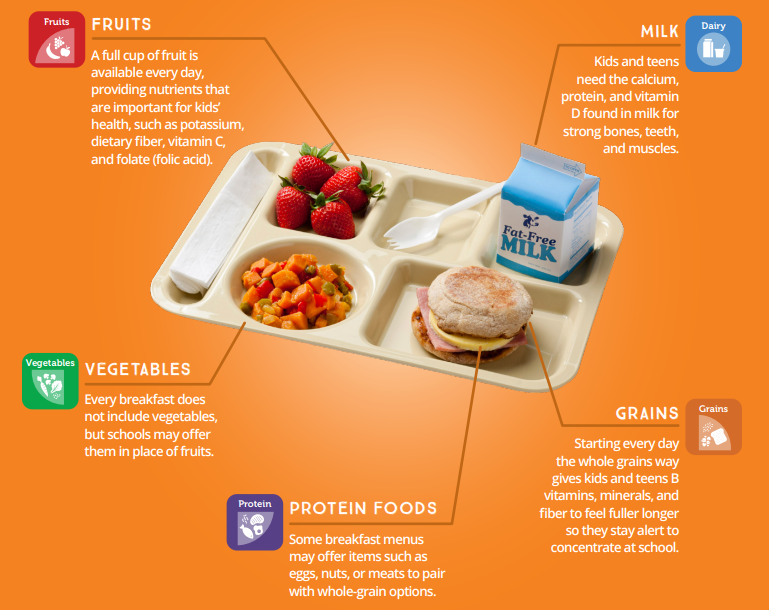
Breakfast
Research has shown that children that eat breakfast do better in school and have higher intakes of fiber, B vitamins, calcium, and other nutrients.[47] Refer to Figure 14.7 to see what a school breakfast includes.
Lunch
Lunch is important because it meets 1/3 of the nutritional needs of most children for the day. And kids with healthier eating patterns have better academic performance.[48]

Meals and Snacks in School-Aged Care Programs
On school days, children that are in care before school may need to be fed breakfast (if they did not eat at home or will not be eating at school). After school, they will need substantial, healthy snacks. On full days of care, they will need breakfast, lunch, and a snack.
Follow the menu planning advice in Chapter 15. And involve the children in menu planning and food preparation whenever possible and see which of the suggestions in the following feature for families might also be incorporated into the classroom.
Activities Families Can Do with Children
Choosemyplate.gov offers some fun ideas for families to teach their children about healthy eating and engage the whole family in making healthy choices. Some of these include:
- Food critic game where children select a new food to try and rate it on visual appeal, smell, taste, and texture.[52]
- Grocery store bingo where children identify foods they see in the grocery store to try to get a 5 in a row bingo.[53]
- Make food visually appealing by turning it into art.
- Kid’s Restaurant: Kids get to plan out the meal, design the menu, and prepare the dish.
- Growing a garden (or starting small with an herb box in a window).
- Going to a local farmer’s market or farm stand to find local food options to buy, take home, and turn into a delicious meal.
Making Mealtimes Fun
Here are some tips for families for making mealtimes more relaxed and enjoyable:
- Remove distractions, such as phones, tablets, and turn off the television.
- Have conversations. Use starters like:
- Give each family member the spotlight to share their highlight, lowlight, and “funnylight”
- If our family lived in a zoo, what animals would we be and why?
- If you could have one superpower, what would it be and why?
- If you were stranded on a desert island and could only have one food to eat, what would it be and why?
- Pass on traditions, both the foods and the stories behind them.
- Let the children make the choices (from a healthy selection of foods).
- Let everyone help prepare and clean up after meals.
- Consider a change of scenery, like a picnic.
- Reserve a special plate to rotate between family members, for example on birthdays, when someone gets a good grade, or any other occasion you’d like to recognize.[54]
Feeding Children with Special Needs
Some disabilities and other exceptional needs may affect children’s nutrition. For example:
- Children with cerebral palsy or cystic fibrosis may have different caloric needs.
- Children with celiac disease or irritable bowel syndrome may have dietary restrictions.
- Children with cleft lip or palate may have physical difficulties with eating.
- Children on the autism spectrum may have strong food preferences or aversions.

Because each child’s specific needs will vary, early care and education programs should work closely with families, and medical providers as needed, to ensure that they understand and can meet the nutritional and feeding needs of the individual child (not a generalization or assumption about the child might need based on a diagnosis or label).
Nutrition policies and practices should be created to be inclusive of children with special needs. Some general considerations early care and education programs and schools should make to ensure that all children’s nutritional needs are met and that all children experience positive meal and snack times include:
- Ensure that the spaces in which children eat and access to drinking water are fully accessible to all children, including those with mobility impairments (and if needed, assistive devices should be provided).
- Staff should be trained to provide for children who may have additional or differing nutritional or feeding needs so they can work effectively and comfortably with all children.
- Follow any dietary restrictions.[56]
Summary
Early care and education programs can provide for all children’s nutrition when they understand:
- The general changes children have in nutritional needs as they mature,
- Common challenges across the different stages of development, and
- Strategies that foster positive meal and snack times at each age stage, and
- The fact that children may have diverse and unique nutritional needs
Programs also play an important role in children’s nutrition by empowering families by providing support, information, and resources as they make decisions about how to feed their children.
Chapter 14 Review
Resources for Further Exploration
- Head Starts’ Growing Healthy guide
- Ellyn Satter Institute
- USDA’s Breastfeeding: Why Not Give It a Try?
- Toddler Nutrition and Health Resource List
- Resources on MyPlate.gov
- Daily Food Plan
- Preschoolers
- Kids
- Healthy Beverages in Early Care and Education
- The CDC Guide to Strategies to Support Breastfeeding Mothers and Babies
- KidsHealth From Nemours Nutrition & Fitness Center
- USDA’s Accommodating Children with Special Dietary Needs in the School Nutrition Programs
- USDA’s Nutrition Curricula
- Golisano Children’s Hospital’s Special Diets for Nutritional Special Needs
References:
[1] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[2] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[3] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[4] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[5] The Important Role of Staff in Breastfeeding Education and Support by Head Start Early Childhood Learning & Knowledge Center is in the public domain
[6] Breastfed Babies Welcome Here! by the USDA Food and Nutrition Service is in the public domain
[7] Nellis Child Development Center II by Staff Sgt. Taylor Worley (USAF) is in the public domain
[8] Breastfed Babies Welcome Here! by the USDA Food and Nutrition Service is in the public domain
[9] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[10] Image by Ben Kerckx on Pixabay
[11] Breastfed Babies Welcome Here! by the USDA Food and Nutrition Service is in the public domain
[12] Healthy Feeding from the Start: A Resource for Expectant Families by the National Center on Early Childhood Health and Wellness is in the public domain
[13] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[14] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[15] Tips for Keeping Infants and Toddlers Safe: A Developmental Guide for Home Visitors – Mobile Infants by Early Head Start National Resource Center is in the public domain
[16] Introducing Complementary Foods: Feeding from Around 6 Months by Queensland Government is licensed under CC BY 4.0
[17] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[18] Feeding Patterns and Diet – Children 6 Months to 2 Years by MedlinePlus is in the public domain
[19] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[20] Tips for Keeping Infants and Toddlers Safe: A Developmental Guide for Home Visitors – Mobile Infants by Early Head Start National Resource Center is in the public domain
[21] Feeding Patterns and Diet – Children 6 Months to 2 Years by MedlinePlus is in the public domain
[22] Tips for Keeping Infants and Toddlers Safe: A Developmental Guide for Home Visitors – Mobile Infants by Early Head Start National Resource Center is in the public domain
[23] Image by the National Center on Early Childhood Health and Wellness is in the public domain
[24] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[25] Growing Healthy by the National Center on Early Childhood Health and Wellness is in the public domain
[26] Growing Healthy by the National Center on Early Childhood Health and Wellness is in the public domain
[27] Infant and Newborn Nutrition by MedlinePlus is in the public domain
[28] Feeding Patterns and Diet – Children 6 Months to 2 Years by MedlinePlus is in the public domain
[29] Growing Healthy by the National Center on Early Childhood Health and Wellness is in the public domain
[30] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[31] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[32] Image by the National Center on Early Childhood Health and Wellness is in the public domain
[33] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[34] Feeding Your Toddler by Head Start Early Childhood Learning & Knowledge Center is in the public domain
[35] Feeding Your Toddler by Head Start Early Childhood Learning & Knowledge Center is in the public domain
[36] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[37] Serving Spoons and Healthy Habits by Mallory Feeney is in the public domain
[38] How Much Does My Preschooler Need? by the USDA Center for Nutrition Policy and Promotion is in the public domain
[39] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[40] Tips for Picky Eaters by the USDA Center for Nutrition Policy and Promotion is in the public domain
[41] Tips for Picky Eaters by the USDA Center for Nutrition Policy and Promotion is in the public domain
[42] Healthy Tips for Picky Eaters by the USDA Center for Nutrition Policy and Promotion is in the public domain
[43] Healthy Eating for Preschoolers by the USDA Center for Nutrition Policy and Promotion is in the public domain
[44] Tips for Picky Eaters by the USDA Center for Nutrition Policy and Promotion is in the public domain
[45] Dietary Guidelines for Americans 2015–2020 Appendix 2. Estimated Calorie Needs per Day, by Age, Sex, and Physical Activity Level by the Office of Disease Prevention and Health Promotion is in the public domain
[46] Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0
[47] MyPlate Guide to School Breakfast for Families by the USDA Center for Nutrition Policy and Promotion is in the public domain
[48] MyPlate Guide to School Breakfast for Families by the USDA Center for Nutrition Policy and Promotion is in the public domain
[49] Image by the USDA Center for Nutrition Policy and Promotion is in the public domain
[50] Image by the USDA Center for Nutrition Policy and Promotion is in the public domain
[51] Schriever Children Learn New Skills at Cooking Camp by 2nd Lt. Idalí Beltré Acevedo (USAF) is in the public domain
[52] Kids Food Critic Activity by the USDA Center for Nutrition Policy and Promotion is in the public domain
[53] MyPlate Grocery Store Bingo by the USDA Center for Nutrition Policy and Promotion is in the public domain
[54] MyPlate, MyWins for Families by the USDA Center for Nutrition Policy and Promotion is in the public domain
[55] Cleft Nurser Mead Johnson by King97tut is in the public domain

