10 Children with Special Health Care Needs
Learning Objectives
By the end of this chapter, you should be able to:
- Relate family-centered care and individualized planning and care.
- Explain what individualized health planning is and who it is appropriate for.
- Describe some chronic health conditions that children in early care and education programs may have.
- Discuss what inclusion is and why it is beneficial.
Introduction
Children with special health care needs are defined as “. . . those who have or are at increased risk for a chronic physical, developmental, behavioural, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally” (McPherson, 1998).
Any child who meets these criteria in an early care and education setting should have an up-to-date care plan, completed by their primary health care provider with input from parents/guardians, included in their on-site health record and readily accessible to those caring for the child.[1]
Individualized Planning for Health
What does it take to care for children with chronic conditions in an early care and education program? There’s no single recipe for all situations. What it takes—more than any policy, list of services, or staffing plan—is a commitment to communication, collaboration, and creative problem-solving, and a determination to make it work. The essential principles that should guide the care of children with chronic conditions in early childhood education are: care should be family-centered, individualized, safe, and legal.
Family-Centered Care
Over the last 15 years, children’s health care and the relationship between families and health professionals have changed significantly. The role of parents/caregivers has shifted from being patients to partners with the health care provider; and the “good patient” has changed from unquestioningly following advice to being a good partner who actively participates in decisions and advocates for services for their child.

“Family-centered care” involves providing the family health care and other services based on the family’s needs, priorities, and convenience rather than those of the service providers or the child alone. Family-centered services are evidence of a program’s commitment to family partnerships and supporting child and family development.
Services are family-centered when:
- The family is recognized as the child’s most constant and important caregiver.
- The family and professionals collaborate as partners.
- Communication is open and honest, in both directions, between the family and professionals.
- Individual strengths and differences are respected among families.
- Services are flexible and responsive to the family’s needs.
- Family-to-family support is encouraged.
- Children with chronic conditions and their families are treated like other children and families, and not defined by their condition.
Individualizing Care
Individualizing means recognizing the characteristics that make each child unique and planning a program that responds to these differences. Individualizing allows families and staff to respond to each child’s built-in time clock for development, as well as culture, family, home language, life experiences, strengths, needs, skills, and abilities.
Early care and education programs can best meet the needs of children with chronic conditions by following a systematic process of Individualized Health Planning. For children who are eligible for an Individualized Education Program (IEP) or Individualized Family Service Plan (IFSP), the IEP or IFSP may or may not include planning for the child’s health care needs. In addition, many children with special health needs who are not eligible for an IEP or IFSP would, in fact, benefit from individualized health planning.
Individualized health planning for children with chronic conditions involves close communication and collaboration among families, the early care and education program staff, and health care and service providers. It is a process of collecting all the necessary information from screening and evaluations, developing plans for the child’s routine and emergency care, conducting ongoing assessment, and revising the plans as needed. The plan should be documented in writing to serve as a clear guide for staff, families, and health care providers on meeting the child’s health needs.
Who Should Have an Individualized Health Plan?
Children who would benefit from an Individualized Health Plan include any child who:
- Requires adaptations in daily activities because of a medical condition; daily activities to be considered include feeding, playing, sleeping, toileting.
- Needs medication regularly.
- Requires a specialized emergency plan.
The decision to develop an Individualized Health Plan for a child should be made collaboratively by the family, health specialists, and classroom teacher.
What are the Benefits of an Individualized Health Plan?
- Health Promotion and Prevention of Complications: Children with chronic conditions remain healthiest when all possible measures are taken to promote their general health and manage the chronic condition closely.
- Communication and Collaboration: Optimal health care for children with chronic conditions requires close communication and coordination among families, Head Start, and health care providers.

Figure 10.2 – Families, health care and service providers, and early care and education programs can work together to make sure children with special health needs get the care they need. - Training and Skills: An Individualized Health Plan identifies the specific procedures needed to care for a child with chronic conditions.
- Confidence: With an Individualized Health Plan, families and program staff can feel confident that they are doing everything possible to keep the child healthy on a routine and daily basis. Also, if health problems or emergencies occur, they can feel confident that they are prepared to manage them in the best way possible. Children with special medical needs feel more secure and able to learn when their caregivers know what to do.
What should be Included in an Individualized Health Plan?
Caring for children with chronic conditions is a serious responsibility. Staff are commonly concerned about meeting the child’s daily care needs: “How can I be sure to give him his medicine at the right time? Do we have enough staff to do his tracheostomy care while also supervising the other children? Will I have all his asthma supplies on the field trip?” Staff are also commonly concerned about emergencies: “What if I give her the wrong amount of medicine? What if she stops breathing? What if I can’t reach her father on the phone?” The Individualized Health Plan should include the information necessary to respond to the most likely “what-ifs.”
Many people are afraid to care for children with chronic conditions. It can raise anxieties to discuss and plan for the “what-if” situations. It is important to remember that anticipating and planning for a situation doesn’t make it happen; it just allows you to be prepared if it does.
At minimum, an Individualized Health Plan should be a guide to:
- What accommodations in daily programming are needed, including meals and snacks, playing, sleeping, and toileting.
- When and how to give medication, and who may give it.
- When and how to perform any required medical procedures, and who may perform them.
- What procedures to follow in the event of a medical emergency.
The Individualized Health Plan should be developed with the participation of families, medical professionals, classroom staff, and any other program that may be involved in providing care. All parties should sign the form as an indication of agreement with and commitment to plan.[4] See the example of a health plan in Appendix M.
Who are Children with Special Needs?
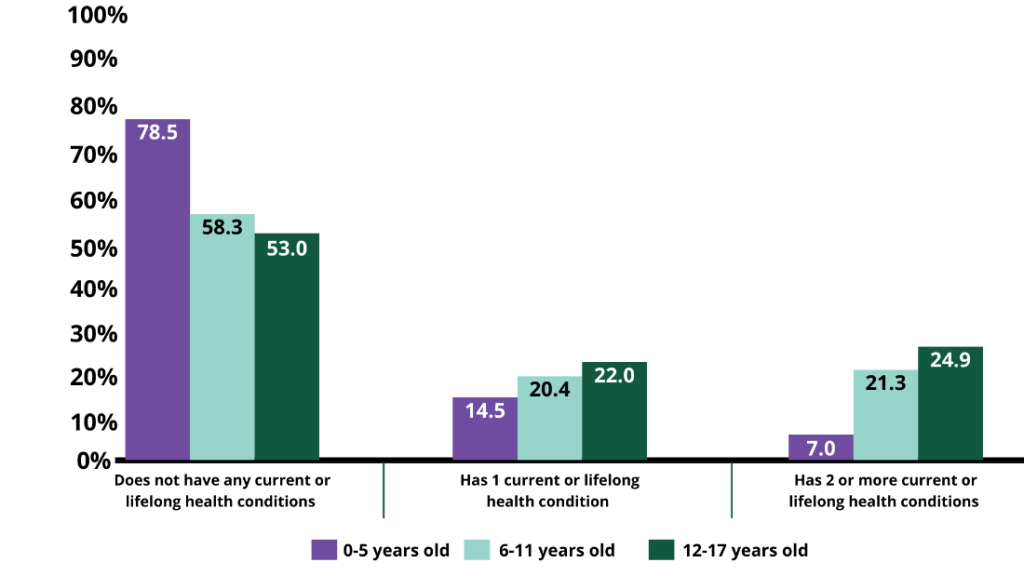
According to Data Resource Center for Child and Adolescent Health and shown in Figure 10.3, in 2017 over 20% of children 0-5 years, and over 40% of children 6-11 years, have one or more of the following current or lifelong health conditions:
- Allergies (food, drug, insect or other)
- Arthritis
- Asthma
- Blood disorders (such as sickle cell disease, thalassemia, or hemophilia)
- Brain injury/concussion/head injury
- Cerebral palsy
- Cystic fibrosis
- Diabetes
- Down Syndrome
- Epilepsy or seizure disorder
- Genetic or inherited condition
- Heart condition
- Frequent or severe headaches including migraine (3-17 years)
- Tourette Syndrome (3-17 years)
- Anxiety problems (3-17 years)
- Depression (3-17 years)
- Behavioural and conduct problem (3-17 years)
- Substance use disorder (6-17 years)
- Developmental delay (3-17 years)
- Intellectual disability (3-17 years)
- Speech or other language disorder (3-17 years)
- Learning disability (also known as mental retardation) (3-17 years)
- Other mental health condition (3-17 years)
- Autism or Autism Spectrum Disorder (ASD) (3-17 years)
- Attention Deficit Disorder or Attention-Deficit/Hyperactivity Disorder (ADD or ADHD) (3-17 years)
- Hearing problems
- Vision problems. [3]
Introduction to Chronic Health Conditions
Although no summary in a textbook will replace the knowledge families and their health care and service providers can provide about a child who has a chronic health condition, it can be helpful to have some familiarity with different conditions. Here is some introductory information on some of the chronic health conditions children in early care and education programs may have.
Allergies
An allergy is a reaction by the immune system to something that does not bother most other people. People who have allergies often are sensitive to more than one thing. Substances that often cause reactions are:
- Pollen
- Dust mites
- Mold spores
- Pet dander
- Food
- Insect stings
- Medicines.
Figure 10.4 – This child suffers from allergies.
Normally, the immune system fights germs. It is the body’s defense system. In most allergic reactions, however, it is responding to a false alarm. Genes and the environment probably both play a role.
Allergies can cause a variety of symptoms such as a runny nose, sneezing, itching, rashes, swelling, or asthma. Allergies can range from minor to severe. Anaphylaxis is a severe reaction that can be life-threatening. Doctors use skin and blood tests to diagnose allergies. Treatments include medicines, allergy shots, and avoiding the substances that cause the reactions. [6]
Key Takeaways
Anaphylaxis
Anaphylaxis is a serious allergic reaction. It can begin very quickly, and symptoms may be life-threatening. The most common causes are reactions to foods (especially peanuts), medications, and stinging insects. Other causes include exercise and exposure to latex. Sometimes no cause can be found.
It can affect many organs:
- Skin – itching, hives, redness, swelling
- Nose – sneezing, stuffy nose, runny nose
- Mouth – itching, swelling of the lips or tongue
- Throat – itching, tightness, trouble swallowing, swelling of the back of the throat
- Chest – shortness of breath, coughing, wheezing, chest pain or tightness
- Heart – weak pulse, passing out, shock
- Gastrointestinal tract – vomiting, diarrhea, cramps
- Nervous system – dizziness or fainting.
If child is having a serious allergic reaction, 911 should be called. If an auto-injector is available, give the injection right away. [7]
Arthritis
Arthritis in children is called childhood arthritis or juvenile arthritis. The most common type of childhood arthritis is juvenile idiopathic arthritis (JIA), also known as juvenile rheumatoid arthritis.
Childhood arthritis can cause permanent physical damage to joints. This damage can make it hard for the child to do everyday things like walking or dressing and can result in disability.
Symptoms may come and go over time. There may be times when symptoms get worse, known as flares, and times when symptoms get better, known as remission. Signs and symptoms include:
- Joint pain
- Swelling
- Fever
- Stiffness
- Rash
- Fatigue (tiredness)
- Loss of appetite
- Inflammation of the eye
- Difficulty with daily living activities such as walking, dressing, and playing.
The exact cause of childhood arthritis is unknown. In childhood arthritis, the immune system may not work right which causes the inflammation in the joints and other body systems. Although there is no cure, some children with arthritis achieve permanent remission, which means the disease is no longer active. Any physical damage to the joint will remain. [8]
Asthma
Asthma is a disease that affects the lungs. In the United States, about 20 million people have asthma. Nearly 9 million of them are children. Children have smaller airways than adults, which makes asthma especially serious for them. [9] It causes wheezing, breathlessness, chest tightness, and coughing at night or early in the morning. If a person has asthma, they have it all the time, but they will have asthma attacks only when something bothers their lungs.
An asthma attack may include coughing, chest tightness, wheezing, and trouble breathing. The attack happens in the body’s airways, which are the paths that carry air to the lungs. As the air moves through the lungs, the airways become smaller, like the branches of a tree are smaller than the tree trunk. During an asthma attack, the sides of the airways in the lungs swell and the airways shrink. Less air gets in and out of the lungs, and mucous that the body makes clogs up the airways.
An asthma attack can happen when the person is exposed to asthma triggers. Your asthma triggers can be very different from someone else’s asthma triggers. It’s important for teacher to know about the triggers for any child in their care that has asthma, so they can help the child avoid them and watch for an attack when you can’t. [10] Triggers include:
- Allergens – mold, pollen, animals

Figure 10.5 – A child using an inhaler to control asthma. - Irritants – cigarette smoke, air pollution
- Weather – cold air, changes in weather
- Exercise
- Infections – flu, common cold. [11]
Asthma is treated with medication. There are quick-relief and long-term medications. Some are taken orally and some may be breathed it. It’s important to have accurate information in the health plan and in the child’s records about a child with asthma’s medication. [13]
Blood Disorders
There are several blood disorders that children in early care and education programs may have. Here is an introduction to hemophilia, sickle cell disease, and thalassemia.
Hemophilia
Hemophilia is usually an inherited bleeding disorder in which the blood does not clot properly. This can lead to spontaneous bleeding as well as bleeding following injuries or surgery. Blood contains many proteins called clotting factors that can help to stop bleeding. People with hemophilia have low levels of either factor VIII (8) or factor IX (9). The severity of hemophilia that a person has is determined by the amount of factor in the blood. The lower the amount of the factor, the more likely it is that bleeding will occur which can lead to serious health problems.
Hemophilia is caused by a mutation or change, in one of the genes, that provides instructions for making the clotting factor proteins needed to form a blood clot. This change or mutation can prevent the clotting protein from working properly or to be missing altogether. Hemophilia occurs in about 1 of every 5,000 male births. Females can also have hemophilia, but this is much rarer (and more often they are carriers). Hemophilia affects people from all racial and ethnic groups.
The best way to treat hemophilia is to replace the missing blood clotting factor so that the blood can clot properly. This is done by infusing (administering through a vein) commercially prepared factor concentrates. [14]Hemophilia is a complex disorder. Good quality medical care from doctors and nurses who know a lot about the disorder can help people with hemophilia prevent some serious problems. [15]
Sickle Cell Disease
SCD is a group of inherited red blood cell disorders. Healthy red blood cells are round, and they move through small blood vessels to carry oxygen to all parts of the body. In someone who has SCD, the red blood cells become hard and sticky and look like a C-shaped farm tool called a “sickle”. The sickle cells die early, which causes a constant shortage of red blood cells. Also, when they travel through small blood vessels, they get stuck and clog the blood flow. This can cause pain and other serious problems such infection, acute chest syndrome and stroke.
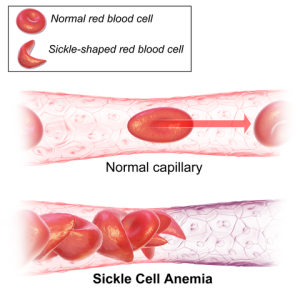
SCD is a genetic condition that is present at birth. It is inherited when a child receives two sickle cell genes—one from each parent. People with SCD start to have signs of the disease during the first year of life, usually around 5 months of age. Symptoms and complications of SCD are different for each person and can range from mild to severe.
There is no single best treatment for all people with SCD. Treatment options are different for each person depending on the symptoms. The only cure for SCD is bone marrow or stem cell transplant.[19]
Thalassemia
Thalassemia is an inherited blood disorder caused when the body doesn’t make enough of a protein called hemoglobin, an important part of red blood cells. When there isn’t enough hemoglobin, the body’s red blood cells don’t function properly and they last shorter periods of time, so there are fewer healthy red blood cells traveling in the bloodstream.
Red blood cells carry oxygen to all the cells of the body. Oxygen is a sort of food that cells use to function. When there are not enough healthy red blood cells, there is also not enough oxygen delivered to all the other cells of the body, which may cause a person to feel tired, weak or short of breath. This is a condition called anemia.
People with thalassemia may have mild or severe anemia. Severe anemia can damage organs and lead to death. People with moderate and severe forms of thalassemia usually find out about their condition in childhood, since they have symptoms of severe anemia early in life. [17]
Symptoms of anemia include:
- Dizziness
- Shortness of breath
- A fast heart beat
- Headache
- Leg cramps
- Difficulty concentrating
- Pale skin.
The type of treatment a person receives depends on how severe the thalassemia is. The more severe the thalassemia, the less hemoglobin the body has, and the more severe the anemia may be. One way to treat anemia is to provide the body with more red blood cells to carry oxygen. This can be done through a blood transfusion, a safe, common procedure in which the person receives blood through a small plastic tube inserted into one of their blood vessels. [18]
Cerebral Palsy
Cerebral palsy (CP) is a group of disorders that affect a person’s ability to move and maintain balance and posture. CP is the most common motor disability in childhood. Cerebral means having to do with the brain. Palsy means weakness or problems with using the muscles. CP is caused by abnormal brain development or damage to the developing brain that affects a person’s ability to control his or her muscles.
The symptoms of CP vary from person to person. A child with severe CP might need to use special equipment to be able to walk, or might not be able to walk at all and might need lifelong care. A child with mild CP, on the other hand, might walk a little awkwardly, but might not need any special help. CP does not get worse over time, though the exact symptoms can change over a person’s lifetime.
All people with CP have problems with movement and posture. Many also have related conditions such as intellectual disability; seizures; problems with vision, hearing, or speech; changes in the spine (such as scoliosis); or joint problems (such as contractures).

Doctors classify CP according to the main type of movement disorder involved. Depending on which areas of the brain are affected, one or more of the following movement disorders can occur:
- Stiff muscles (spasticity)
- Uncontrollable movements (dyskinesia)
- Poor balance and coordination (ataxia).
There is no cure for CP, but treatment can improve the lives of those who have the condition. It is important to begin a treatment program as early as possible.
After a CP diagnosis is made, a team of health professionals works with the child and family to develop a plan to help the child reach his or her full potential. Common treatments include medicines; surgery; braces; and physical, occupational, and speech therapy. No single treatment is the best one for all children with CP. [20]
Cystic Fibrosis
Cystic fibrosis (CF) is an inherited disease of the mucus and sweat glands. It affects mostly the lungs, pancreas, liver, intestines, sinuses, and sex organs. CF causes mucus to be thick and sticky. The mucus clogs the lungs, causing breathing problems and making it easy for bacteria to grow. This can lead to repeated lung infections and lung damage. [21]It is one of the most common chronic lung diseases in children and young adults. It is a life-threatening disorder.

The symptoms and severity of CF can vary. Some people have serious problems from birth. Others have a milder version of the disease that doesn’t show up until they are teens or young adults.
CF is diagnosed through various tests, such as gene, blood, and sweat tests. There is no cure for CF, but treatments have improved greatly in recent years. In the past, most deaths from CF were in children and teenagers. Today, with improved treatments, some people who have CF are living into their forties, fifties, or older. Treatments may include chest physical therapy, nutritional and respiratory therapies, medicines, and exercise. [23]
Diabetes
Until recently, the common type of diabetes in children and teens was type 1. It was called juvenile diabetes. With Type 1 diabetes, the pancreas does not make insulin. Insulin is a hormone that helps glucose, or sugar, get into your cells to give them energy. Without insulin, too much sugar stays in the blood.
Now younger people are also getting type 2 diabetes. Type 2 diabetes used to be called adult-onset diabetes. But now it is becoming more common in children and teens, due to more obesity. With Type 2 diabetes, the body does not make or use insulin well.
Children have a higher risk of type 2 diabetes if they are overweight or have obesity, have a family history of diabetes, or are not active. Children who are African American, Hispanic, Native American/Alaska Native, Asian American, or Pacific Islander also have a higher risk. To lower the risk of type 2 diabetes in children
- Have them maintain a healthy weight.
- Be sure they are physically active.
- Have them eat smaller portions of healthy foods.
- Limit time with the TV, computer, and video.
Children and teens with type 1 diabetes may need to take insulin. Type 2 diabetes may be controlled with diet and exercise. If not, patients will need to take oral diabetes medicines or insulin. [24]
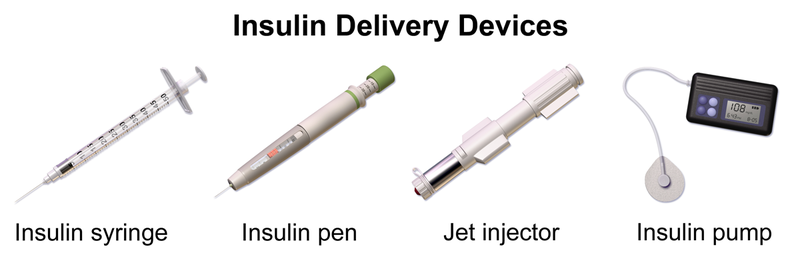
When a child in an early care and education program has type 1 diabetes, staff will be involved in diabetes care on a day-to-day basis, from serving healthy foods to giving insulin injections to watching for and treating hypoglycemia (low blood sugar). [26][/footnote]
Hypoglycemia
Hypoglycemia (low blood sugar) can happen quickly and needs to be treated immediately. It’s most often caused by too much insulin, waiting too long for a meal or snack, not eating enough, or getting extra physical activity. Hypoglycemia symptoms are different from person to person; make sure you know your specific symptoms, which could include:
- Shakiness
- Nervousness or anxiety
- Sweating, chills, or clamminess
- Irritability or impatience
- Dizziness and difficulty concentrating
- Hunger or nausea
- Blurred vision
- Weakness or fatigue
- Anger, stubbornness, or sadness. [27]
Down Syndrome
Down syndrome is a condition in which a person has an extra chromosome. Chromosomes are small “packages” of genes in the body. They determine how a baby’s body forms during pregnancy and how the baby’s body functions as it grows in the womb and after birth. Typically, a baby is born with 46 chromosomes. Babies with Down syndrome have an extra copy of one of these chromosomes, chromosome 21. A medical term for having an extra copy of a chromosome is ‘trisomy.’ Down syndrome is also referred to as Trisomy 21. This extra copy changes how the baby’s body and brain develop, which can cause both mental and physical challenges for the baby.
Even though people with Down syndrome might act and look similar, each person has different abilities. People with Down syndrome usually have an IQ (a measure of intelligence) in the mildly-to-moderately low range and are slower to speak than other children.
Some common physical features of Down syndrome include:
- A flattened face, especially the bridge of the nose
- Almond-shaped eyes that slant up
- A short neck
- Small ears
- A tongue that tends to stick out of the mouth
- Tiny white spots on the iris (coloured part) of the eye
- Small hands and feet
- A single line across the palm of the hand (palmar crease)
- Small pinky fingers that sometimes curve toward the thumb
- Poor muscle tone or loose joints
- Shorter in height as children and adults.
Many people with Down syndrome have the common facial features and no other major birth defects. However, some people with Down syndrome might have one or more major birth defects or other medical problems. Some of the more common health problems among children with Down syndrome are listed below.
- Hearing loss
- Obstructive sleep apnea, which is a condition where the person’s breathing temporarily stops while asleep
- Ear infections
- Eye diseases
- Heart defects present at birth.

Down syndrome is a lifelong condition. Services early in life will often help babies and children with Down syndrome to improve their physical and intellectual abilities. Most of these services focus on helping children with Down syndrome develop to their full potential. These services include speech, occupational, and physical therapy, and they are typically offered through early intervention programs in each state. Children with Down syndrome may also need extra help or attention in early care and education programs and school, although many children are included in classrooms with children that do not have special needs.[28]
Epilepsy (Seizure disorders)
Epilepsy is a broad term used for a brain disorder that causes seizures. There are many different types of epilepsy. There are also different kinds of seizures. [29]A seizure is a short change in normal brain activity. Seizures are the main sign of epilepsy. Some seizures can look like staring spells. Other seizures cause a person to fall, shake, and lose awareness of what’s going on around them. [30]
Most seizures end in a few minutes. If a child has a seizure the teacher should:
- Stay with the child until the seizure ends and he or she is fully awake. Once they are alert and able to communicate, tell them what happened in very simple terms.
- Comfort the person and speak calmly.
- Keep yourself and other people calm.
- Follow the directions in the Health Care Plan (which likely will include calling the family)
Teacher should never do any of the following things:

- Do nothold the child down or try to stop their movements.
- Do notput anything in the child’s mouth. This can injure teeth or the jaw. A person having a seizure cannot swallow his or her tongue.
- Do nottry to give mouth-to-mouth breaths (like CPR). People usually start breathing again on their own after a seizure.
- Do not offer the person water or food until he or she is fully alert. [31]
Nationwide, about 470,000 children have epilepsy. For many children, epilepsy is easily controlled with medicine. These children can do what other kids can do, and perform as well in school. For others, it can be more challenging. [33]
Attention-Deficit/Hyperactivity Disorder (ADHD)
ADHD is one of the most common neurodevelopmental disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. Children with ADHD may have trouble paying attention, controlling impulsive behaviours (may act without thinking about what the result will be), or be overly active.
It is normal for children to have trouble focusing and behaving at one time or another. However, children with ADHD do not just grow out of these behaviours. The symptoms continue, can be severe, and can cause difficulty at school, at home, or with friends.
A child with ADHD might:
- Daydream a lot
- Forget or lose things a lot
- Squirm or fidget
- Talk too much
- Make careless mistakes or take unnecessary risks
- Have a hard time resisting temptation
- Have trouble taking turns
- Have difficulty getting along with others.
There are three different types of ADHD, depending on which types of symptoms are strongest in the individual. Because symptoms can change over time, the presentation may change over time as well.
Predominantly Inattentive Presentation: It is hard for the individual to organize or finish a task, to pay attention to details, or to follow instructions or conversations. The person is easily distracted or forgets details of daily routines.
Predominantly Hyperactive-Impulsive Presentation: The person fidgets and talks a lot. It is hard to sit still for long (e.g., for a meal or while doing homework). Smaller children may run, jump or climb constantly. The individual feels restless and has trouble with impulsivity. Someone who is impulsive may interrupt others a lot, grab things from people, or speak at inappropriate times. It is hard for the person to wait their turn or listen to directions. A person with impulsiveness may have more accidents and injuries than others.
Combined Presentation: Symptoms of the above two types are equally present in the person.
The cause(s) and risk factors for ADHD are unknown, but current research shows that genetics plays an important role. Recent studies of twins link genes with ADHD. In addition to genetics, scientists are studying other possible causes and risk factors including:
- Brain injury
- Exposure to environmental (e.g., lead) during pregnancy or at a young age
- Alcohol and tobacco use during pregnancy
- Premature delivery
- Low birth weight.
Research does not support the popularly held views that ADHD is caused by eating too much sugar, watching too much television, parenting, or social and environmental factors such as poverty or family chaos.
For preschool-aged children (4-5 years of age) with ADHD, behaviour therapy, particularly training for parents, is recommended as the first line of treatment before medication is tried. What works best can depend on the child and family. Good treatment plans will include close monitoring, follow-ups, and making changes, if needed, along the way. [34]
Autism Spectrum Disorder (ASD)
Autism spectrum disorder (ASD) is a developmental disability that can cause significant social, communication and behavioural challenges. There is often nothing about how people with ASD look that sets them apart from other people, but people with ASD may communicate, interact, behave, and learn in ways that are different from most other people. A diagnosis of ASD now includes several conditions that used to be diagnosed separately: autistic disorder, pervasive developmental disorder not otherwise specified (PDD-NOS), and Asperger syndrome. These conditions are now all called autism spectrum disorder.
The learning, thinking, and problem-solving abilities of people with ASD can range from gifted to severely challenged. Some people with ASD need a lot of help in their daily lives; others need less. People with ASD might repeat certain behaviours and might not want change in their daily activities. Many people with ASD also have different ways of learning, paying attention, or reacting to things. Signs of ASD begin during early childhood and typically last throughout a person’s life.

Children or adults with ASD might:
- Not point at objects to show interest (for example, not point at an airplane flying over).
- Not look at objects when another person points at them.
- Have trouble relating to others or not have an interest in other people at all.
- Avoid eye contact and want to be alone.
- Have trouble understanding other people’s feelings or talking about their own feelings.
- Prefer not to be held or cuddled, or might cuddle only when they want to.
- Appear to be unaware when people talk to them, but respond to other sounds.
- Be very interested in people, but not know how to talk, play, or relate to them.
- Repeat or echo words or phrases said to them, or repeat words or phrases in place of normal language.
- Have trouble expressing their needs using typical words or motions.
- Not play “pretend” games (for example, not pretend to “feed” a doll).
- Repeat actions over and over again.
- Have trouble adapting when a routine changes.
- Have unusual reactions to the way things smell, taste, look, feel, or sound.
- Lose skills they once had (for example, stop saying words they were using).
We do not know all of the causes of ASD. However, we have learned that there are likely many causes for multiple types of ASD. There may be many different factors that make a child more likely to have an ASD, including environmental, biologic and genetic factors. ASD occurs in all racial, ethnic, and socioeconomic groups, but is about 4 times more common among boys than among girls.
Research shows that early intervention treatment services can improve a child’s development. Services can help the child meet developmental milestones and interact with others. There is no cure for ASD. [35]But not everyone believes that autism is a condition or disorder or that it needs to be cured.
Neurodiversity
“Neurodiversity is a concept that’s been around for a while. In a nutshell, it means that brain differences are just that: differences. So conditions like ADHD and [ASD] aren’t “abnormal.” They’re simply variations of the human brain.
For kids with learning and thinking differences, the idea of neurodiversity has real benefits. It can help kids (and their parents) frame their challenges as differences, rather than as deficits. It can also shed light on instructional approaches that might help to highlight particular strengths kids have.”[36]
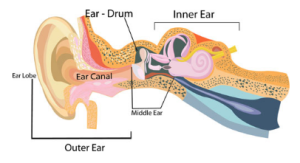
Hearing Problems
Hearing loss can happen when any part of the ear is not working in the usual way. This includes the outer ear, middle ear, inner ear, hearing (acoustic) nerve, and auditory system.
- The outer ear is made up of:
-
- The part we see on the sides of our heads, known as pinna.
- The ear canal.
- The eardrum, sometimes called the tympanic membrane, which separates the outer and middle ear.
- The middle ear is made up of:
-
- The eardrum.
- Three small bones called ossicles that send the movement of the eardrum to the inner ear.
- The inner ear is made up of:
-
- The snail shaped organ for hearing known as the cochlea.
- The semicircular canals that help with balance.
- The nerves that go to the brain.
- The auditory (ear) nerve sends sound information from the ear to the brain.
- The auditory (hearing) system processes sound information as it travels from the ear to the brain so that our brain pathways are part of our hearing.
There are four types of hearing loss:
- Conductive Hearing Loss: Hearing loss caused by something that stops sounds from getting through the outer or middle ear. This type of hearing loss can often be treated with medicine or surgery.
- Sensorineural Hearing Loss : Hearing loss that occurs when there is a problem in the way the inner ear or hearing nerve works.
- Mixed Hearing Loss: Hearing loss that includes both a conductive and a sensorineural hearing loss.
- Auditory Neuropathy Spectrum Disorder: Hearing loss that occurs when sound enters the ear normally, but because of damage to the inner ear or the hearing nerve, sound isn’t organized in a way that the brain can understand.
The degree of hearing loss can range from mild to profound:
- Mild Hearing Loss: A person with a mild hearing loss may hear some speech sounds but soft sounds are hard to hear.
- Moderate Hearing Loss: A person with a moderate hearing loss may hear almost no speech when another person is talking at a normal level.
- Severe Hearing Loss: A person with severe hearing loss will hear no speech when a person is talking at a normal level and only some loud sounds.
- Profound Hearing Loss: A person with a profound hearing loss will not hear any speech and only very loud sounds. [38]
Hearing loss can happen any time during life – from before birth to adulthood. Following are some of the things that can increase the chance that a child will have hearing loss:
- A genetic cause: About 1 out of 2 cases of hearing loss in babies is due to genetic causes.
- 1 out of 4 cases of hearing loss in babies is due to maternal infections during pregnancy, complications after birth, and head trauma.
- For about 1 out of 4 babies born with hearing loss, the cause is unknown.
Hearing loss can affect a child’s ability to develop speech, language, and social skills. The earlier children with hearing loss start getting services, the more likely they are to reach their full potential. [39] Screening for hearing loss was covered in Chapter 7.
Vision Problems
In Canada, common vision disorders include amblyopia, strabismus, and significant refractive errors. Early detection increases the likelihood of effective treatment. [46] Vision screening was also addressed in Chapter 7.
Amblyopia
Amblyopia, also referred to as “lazy eye,” is the most common cause of vision impairment in children. Amblyopia is the medical term used when the vision in one of the eyes is reduced because the eye and the brain are not working together properly.

The eye itself looks normal, but it is not being used normally because the brain is favouring the other eye. Conditions leading to amblyopia include strabismus, an imbalance in the positioning of the two eyes, being more nearsighted, farsighted, or astigmatic in one eye than the other eye, and rarely, other eye conditions, such as cataracts.
Unless it is successfully treated in early childhood amblyopia usually persists into adulthood, and is the most common cause of permanent one-eye vision impairment among children and young and middle-aged adults. An estimated 2%–3% of the population suffer from amblyopia.
Strabismus
Strabismus involves an imbalance in the positioning of the two eyes. Strabismus can cause the eyes to cross in (esotropia) or turn out (exotropia). Strabismus is caused by a lack of coordination between the eyes. As a result, the eyes look in different directions and do not focus simultaneously on a single point. In most cases of strabismus in children, the cause is unknown. In more than half of these cases, the problem is present at or shortly after birth (congenital strabismus). When the two eyes fail to focus on the same image, there is reduced or absent depth perception and the brain may learn to ignore the input from one eye, causing permanent vision loss in that eye (one type of amblyopia).
Refractive Errors
Refractive errors in children include myopia (near-sightedness), hyperopia (farsightedness), and astigmatism (distorted vision at all distances), can be corrected by eyeglasses, contact lenses, or in some cases surgery. [40]

Other Eye Diseases
Other eye diseases affecting this age group include retinopathy of prematurity (ROP), congenital defects, diabetic retinopathy (DR), and cancers such as retinoblastoma. [42]
Watch for signs of a vision problem. [43]
Some common signs that a child may be having trouble with their eyes include:
- Squinting or holding objects very close to their face.
- Difficulty seeing and identifying distant objects.
- Losing their place when reading.
- Jerky eye movements.
- Tilting their head.
- Rubbing their eyes.
- Sensitivity to lights.
- Poor hand-eye coordination.
- Having difficulty telling similar colours apart (usually red and green or blue and yellow).
Pause to Reflect
Do you have experiences with any of the special needs discussed in this section?
- How does this affect how you feel about that particular need?
- Did you find yourself feeling more concerned about potentially caring for a child with any of these?
- If so, why?
- What can you do to address those concerns?
- Are there any you feel more comfortable and/or qualified to handle? Why or why not?
Children with Special Needs
Children in early care and education programs may have special needs that are not directly related to their health. The number of children enrolled in Special Education according to the California Department of Education, in the 2018-2019 academic year is provided by disability in Table 10.1. [44]
| Table 10.1 Special Education Entrollment by Age and Disability | |||||||||||||
| Age | ID | HH | Deaf | SLI | VI | ED | OI | OHI | SLD | DB | MD | ASD | TBI |
| 0 | 53 | 334 | 62 | 12 | 23 | 0 | 63 | 288 | 0 | – | 28 | 0 | – |
| 1 | 115 | 605 | 93 | 178 | 72 | 0 | 171 | 764 | 0 | – | 79 | – | – |
| 2 | 134 | 589 | 89 | 860 | 97 | 0 | 137 | 1091 | – | – | 112 | 83 | 0 |
| 3 | 805 | 419 | 136 | 13028 | 67 | – | 351 | 997 | 26 | – | 252 | 6100 | 17 |
| 4 | 1016 | 414 | 114 | 18404 | 96 | 16 | 443 | 1274 | 51 | – | 270 | 7976 | 20 |
| 5 | 1362 | 418 | 148 | 20533 | 110 | 83 | 430 | 1742 | 524 | – | 321 | 8437 | 34 |
| 6 | 1777 | 167 | 167 | 23784 | 140 | 265 | 526 | 3075 | 2339 | – | 349 | 9078 | 40 |
| 7 | 1924 | 170 | 170 | 22053 | 160 | 580 | 549 | 4676 | 7174 | – | 345 | 9024 | 68 |
| 8 | 2228 | 188 | 188 | 17871 | 191 | 879 | 879 | 6035 | 14717 | – | 394 | 8685- | 70 |
CODE: ID = Intellectual Disability, HH = Hard of Hearing, SLI = Speech or Language Impairment, VI = Visual Impairment, ED = Emotional Disturbance, OI = Orthopedic Impairment, OHI = Other Health Impairment, SLD = Specific Learning Disability, DB = Deaf/Blind, MD = Multiple Disabilities, ASD = Autism Spectrum Disorder, TBI = Traumatic Brain Injury.
These children and their families need a partnership with early care and education staff and other service providers as early as possible because it creates a solid foundation to support optimal development and can reduce the prevalence of ongoing and future challenges. [45]
The Individuals with Disabilities Education Act (IDEA) is the federal law that makes available a free appropriate public education to eligible children with disabilities throughout the nation and ensures special education and related services to those children.

The IDEA governs how states and public agencies provide early intervention, special education, and related services to more than 6.5 million eligible infants, toddlers, children, and youth with disabilities. [46]
For children birth to 3 years, Part C of IDEA Provides early intervention services to children from birth to 3 with special needs. And Individualized Family Service Plan (IFSP) is a written document outlining:
- The early intervention services a child and family will receive.
- The child’s needs; the family’s strengths and choices; and the Early Intervention team’s recommendations.
Once children turn 3, Part B of IDEA (Section 619), provides special education services through the public school system. An Individualized Education Program (IEP) is a written plan that describes:
- The child’s educational goals.
- Services and supports in a school setting. [48]
Inclusion
In IDEA, the word appropriate, refers to providing that educational experience in the least restrictive environment (LRE). LRE requires a continuum of placement options be available to best meet the diverse needs of children with disabilities, and presumes that the first placement option considered for each child with a disability is the regular classroom the child would attend if he or she did not have a disability. [49]The full and active participation of children with disabilities or other special needs in community activities, services, and programs designed for children without disabilities, including child care, is referred to as inclusion. In an inclusive program, if support, accommodations, or modifications are needed to ensure the child’s full, active participation, they are provided appropriately. The participation results in an authentic sense of belonging for the child and family.
Teachers may be reassured to know that:
- Child care providers can successfully include children with disabilities or other special needs in the program while promoting belonging for all children.
- Major modifications to their program or facility probably will not be needed in order to include children with disabilities or other special needs.
- Assistance and support for more significant changes in their program or facility may be available.
- An inclusive child care program is rewarding for all the children, families, and staff in child care programs.[57]
Individualizing Care and Education
When serving an individual child, the provider should focus on the child’s needs, not the disability or its label. Working with the family and the service providers, teachers can provide individualized care and education for the child’s unique needs and strengths, just as they should be doing for each and every child in their classroom.
As each child is unique, so is each child care program. There is no magic formula for making inclusion work beyond the creativity, energy, and interest that most child care providers already bring to their work. Their uniqueness notwithstanding, every program is able to successfully include children with disabilities. And each makes it work child by child, day by day.
Some children need small changes to the curriculum or minor supports in order to get the most out of certain activities. These sorts of things may consist of fairly simple accommodations, such as providing a special place or quiet activity for a child who is unable to participate in large-group activities or making available a special snack for a child who needs to eat more frequently than the typical meal or snack schedule. Other children may require more specific adaptations that might not be readily apparent. A variety of community resources can be helpful in determining what those might be. The family, for example, is always the first and most important guide for what a child might need; after that, an area specialist or a local workshop might be. Beyond the immediate community, a world of literature in books, periodicals, and Web sites devoted to disabilities and inclusion can inform a child care provider about appropriate adaptations for a child with a particular condition or need.

Programs that begin with a high-quality, developmentally appropriate foundation; a positive attitude on the part of the care provider; appropriate adult–child ratios; supportive administrators; and adequate training for the provider will be in a good position to creatively solve problems for a child with disabilities or other special needs, exactly as it does for children who are typically developing. If a child already has an established diagnosis, trained intervention personnel may be available to assist in this process.
One of the biggest roles for a care provider is to facilitate a sense of belonging and inclusion. Several helpful strategies are as follows:
- Start with the assumption that all children are competent.
- Adapt the environment so that it is developmentally appropriate, challenging, and fits the needs and interests of each child.
- While there may be a need to support a child’s mastery of a specific skill, keep the whole child in mind, particularly the child’s social-emotional experience.[59]
Common Modifications, Adaptations, and Supports
Each child is an individual, and modifications, adaptations, accommodations, and supports should be designed with a single child in mind. However, researchers from the Early Childhood Research Institute on Inclusion (ECRII) have found that many changes can be grouped into categories of modifications, summarized in Table 10.2.[60]
| Table 10.2 – Common Modifications, Adaptations, and Supports [61] | ||
| Category of Support | Description | Examples |
| Environmental Support | Alter the physical, social, or temporal environment to promote participation, engagement, and learning. | Use a photo, picture, or object to signal the next activity. Make boundaries for activities (e.g., mark sections of the floor with tape, provide a tray or box lid for art activities). Free surfaces of bumps or smooth them with “lips” and ramps. |
| Materials Adaptation | Modify materials to promote independence. | Add knobs to wooden puzzles. Use fabric self-adhesive closures on dress-up clothes. Place “no-slip” placemats under dishes when children eat or serve themselves. |
| Activity Simplification | Simplify a complicated task by breaking it into smaller parts or reducing the number of steps. | Give a child the materials for a task one piece at a time. Prepare materials for easier use. Replace materials that may be difficult to use with ones that are simpler and can serve the same function. |
| Child Preferences | Capitalize on a child’s favourite activities. | Observe a child’s interests and then provide additional materials or toys that match them. Use the child’s preferred activities, such as music, to support efforts to learn other skills. Find ways to build on a child’s preferred activities when introducing new ideas. |
| Special Equipment | Use adaptive devices to facilitate participation. | Ensure that providers know the proper use of adaptive or medical equipment, such as hearing aids, glasses, or nebulizers. Allow all children to participate in activities by providing appropriate seating or other equipment. Use picture cards or electronic switch-activated speaking devices for children who cannot speak. |
| Adult Support | Employ direct adult intervention to support a child’s efforts. | Assign a primary caregiver to a child so that the assigned adult is able to know the unique needs of the child and ways to support them. Provide direct instruction or guidance to a child while he/she is learning or practicing tasks. Learn specific ways of interacting or communicating with a child, such as sign language. |
| Peer Support | Use classmates as models to help children learn. | Pair a child with a certain disability with a child who does not have that disability during certain activities, ensuring that the child with special needs is sometimes the helper and not always the one being helped. Facilitate children’s interactions and observations of one another in small groups. Teach children specific ways to engage and interact with a child with special needs. |
| Invisible Support | Arrange naturally occurring events to assist inclusion. | Stock the dress-up center or kitchen corner with sufficient items so more children can participate in a popular activity without competition. Assign roles during children’s play, such as having a child with limited mobility be in charge of “pumping gas” as the children riding bikes go by. Comment on children’s play in ways that encourage further interaction. |
Pause to Reflect
How might you explain what inclusion is and why it is good for children and families to the following:
- Someone who thinks they want to be a teacher but doesn’t believe they can handle teaching in an inclusive classroom.
- The family of a child with special needs.
- The family of a child that is having a hard time with changes in the classroom after a child that has a special need joined the class.
- Did your explanations differ? Why or why not?
Summary
All children and their families deserve access to and full inclusion in high-quality early care and education programs. This includes children with special health care and other special needs. Working with families and the health care and service providers, programs can meet each child’s individualized needs. This takes knowledge, planning, and partnership. Inclusive programs are beneficial to everyone, the children with the special needs and their families, the children that do not have the special needs, and the program staff.
Chapter 10 Review
Resources for Further Exploration
- American Academy of Pediatrics (AAP)
- Centers for Disease Control and Prevention (CDC)
- KidsHealth® from Nemours
- National Institute of Health, Medline Plus
- Online Learning Course: Medication Administration in Early Education and Child Care
- Asthma and Allergy Foundation of America
- American Lung Association
- Juvenile Arthritis
- American Academy of Cerebral Palsy and Developmental Medicine
- Cystic Fibrosis Foundation
- American Diabetes Association
- National Association for Down Syndrome
- Epilepsy Foundation
- Attention Deficit Disorder Association
- Autism Society of America
- American Society for Deaf Children
- Children’s Eye Foundation of AAPOS
- Information and Technical Assistance on the American with Disabilities Act, Commonly Asked Questions about Child Care Centers and the Americans with Disabilities Act
- Center for Parent Information and Resources
- Disabilities Services Newsletters
- Center on the Social and Emotional Foundations for Early Learning
- Individualization: Strategies for Teaching Children with Special Needs
- Head Start Center for Inclusion
References:
[1] Care Plan for Children with Special Health Care Needs by Head Start Early Childhood Learning & Knowledge Center is in the public domain
[4] Making It on Our Own: Customizing an Individualized Health Plan [A Learning Activity] by Head Start Early Childhood Learning & Knowledge Center is in the public domain
[19] What is Sickle Cell Disease? by the Centers for Disease Control and Prevention is in the public domain
[31] Image by the California Department of Education is used with permission
[46] Age and Vision Loss by the Centers for Disease Control and Prevention is in the public domain
[47] Image by Jennifer Paris used with permission
[57] Inclusion Works! by the California Department of Education is used with permission
[58] Image by the California Department of Education is used with permission
[59] Inclusion Works! by the California Department of Education is used with permission
[60] Inclusion Works! by the California Department of Education is used with permission
[61] Inclusion Works! by the California Department of Education is used with permission
- Image by California Department of Education. (2012). California Infant/Toddler Curriculum Framework. https://www.cde.ca.gov/sp/cd/re/documents/itcurriculumframework.pdf ↵
- Image of Team Meeting by Bob Cotter is licensed under CC BY-NC 2.0 ↵
- Child and Adolescent Health Measurement Initiative. (n.d.). 2017-2018 National Survey of Children’s Health (NSCH) data query. Retrieved from https://www.childhealthdata.org ↵
- Image by College of the Canyons ZTC Team is based on image from source: Data Resource Center for Child & Adolescent Health. (n.d.). 2017-2018 National Survey of Children’s Health. Retrieved from https://www.childhealthdata.org/browse/survey/results?q=6859&r=1&g=713 ↵
- Image of Tired of allergies by Ste Elmore is licensed under CC BY 2.0 ↵
- MedlinePlus. (2018). Allergy. [public domain]. https://medlineplus.gov/allergy.html ↵
- MedlinePlus. (2016). Anaphylaxis. [public domain]. https://medlineplus.gov/anaphylaxis.html ↵
- Centers for Disease Control and Prevention. (2023). Childhood Arthritis. [public domain]. https://www.cdc.gov/arthritis/types/childhood.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Farthritis%2Fbasics%2Fchildhood.htm ↵
- MedlinePlus. (2024). Asthma in Children. [public domain]. https://medlineplus.gov/asthmainchildren.html#summary ↵
- Centers for Disease Control and Prevention. (2023). Learn How to Control Asthma. [public domain]. https://www.cdc.gov/asthma/faqs.htm ↵
- MedlinePlus. (2024). Asthma in Children. [public domain]. https://medlineplus.gov/asthmainchildren.html#summary ↵
- Image of Treating Kids with Asthma (3) by The U.S. Food and Drug Administration. [public domain]. ↵
- Centers for Disease Control and Prevention. (2023). Learn How to Control Asthma. [public domain]. https://www.cdc.gov/asthma/faqs.htm ↵
- Centers for Disease Control and Prevention. (2023). What is Hemophilia? [public domain]. https://www.cdc.gov/ncbddd/hemophilia/facts.html ↵
- Centers for Disease Control and Prevention. (2023). Treatment of Hemophilia. [public domain]. https://www.cdc.gov/ncbddd/hemophilia/treatment.html ↵
- Image of Sickle Cell Anemia by Blausen Medical Communications is licensed under CC BY-SA 4.0 ↵
- Centers for Disease Control and Prevention. (2023). What is Thalassemia? [public domain]. https://www.cdc.gov/ncbddd/thalassemia/facts.html ↵
- Centers for Disease Control and Prevention. (2023). Thalassemia: Complications and Treatment. [public domain]. https://www.cdc.gov/ncbddd/thalassemia/treatment.html ↵
- Image by California Department of Education. (2012). California Infant/Toddler Curriculum Framework. https://www.cde.ca.gov/sp/cd/re/documents/itcurriculumframework.pdf ↵
- Centers for Disease Control and Prevention. (2024). What is Cerebral Palsy? [public domain]. https://www.cdc.gov/ncbddd/cp/facts.html ↵
- MedlinePlus. (2016). Cystic Fibrosis. [public domain]. https://medlineplus.gov/cysticfibrosis.html ↵
- Image by Stacey Geiger is in the public domain ↵
- MedlinePlus. (2016). Cystic Fibrosis. [public domain]. https://medlineplus.gov/cysticfibrosis.html ↵
- MedlinePlus. (2018). Diabetes in Children and Teens. [public domain]. https://medlineplus.gov/diabetesinchildrenandteens.html ↵
- Image of Insulin Delivery Devices by Blausen Medical Communications is licensed under CC BY-SA 4.0 ↵
- [footnote]Centers for Disease Control and Prevention. (2021). Type 1 Diabetes. [public domain]. https://www.cdc.gov/diabetes/basics/type1.html ↵
- Centers for Disease Control and Prevention. (2021). Type 1 Diabetes. [public domain]. https://www.cdc.gov/diabetes/basics/type1.html ↵
- Centers for Disease Control and Prevention. (2023). Facts about Down Syndrome. [public domain]. https://www.cdc.gov/ncbddd/birthdefects/DownSyndrome.html ↵
- Centers for Disease Control and Prevention. (2020). About Epilepsy. [public domain]. https://www.cdc.gov/epilepsy/about/index.htm ↵
- Centers for Disease Control and Prevention. (2023). Epilepsy in Schools. [public domain]. https://www.cdc.gov/epilepsy/groups/schools.htm ↵
- Centers for Disease Control and Prevention. (2022). Seizure First Aid. [public domain].https://www.cdc.gov/epilepsy/about/first-aid.htm ↵
- Image by Airman 1st Class Austin Harvill [public domain]. ↵
- Centers for Disease Control and Prevention. (2023).Epilepsy in Schools. [public domain]. https://www.cdc.gov/epilepsy/groups/schools.htm ↵
- Centers for Disease Control and Prevention. (2023). What is ADHD? [public domain]. https://www.cdc.gov/ncbddd/adhd/facts.html ↵
- Centers for Disease Control and Prevention. (2022). What is Autism Spectrum Disorder? [public domain]. https://www.cdc.gov/ncbddd/autism/facts.html ↵
- Rosen, P. (n.d.) Neurodiversity: What You Need to Know. Understood. Retrieved from https://www.understood.org/en/friends-feelings/empowering-your-child/building-on-strengths/neurodiversity-what-you-need-to-know ↵
- Image from Centers for Disease Control and Prevention. (2023). Types of Hearing Loss. [public domain]. https://www.cdc.gov/ncbddd/hearingloss/types.html ↵
- Centers for Disease Control and Prevention. (2023). Types of Hearing Loss. [public domain]. https://www.cdc.gov/ncbddd/hearingloss/types.html ↵
- Centers for Disease Control and Prevention. (2023). What is Hearing Loss in Children? [public domain]. https://www.cdc.gov/ncbddd/hearingloss/facts.html ↵
- Centers for Disease Control and Prevention. (2023). Common Eye Disorders and Diseases. [public domain]. https://www.cdc.gov/visionhealth/basics/ced/index.html ↵
- Image by California Department of Education. (2012). California Infant/Toddler Curriculum Framework. https://www.cde.ca.gov/sp/cd/re/documents/itcurriculumframework.pdf ↵
- Centers for Disease Control and Prevention. (2022). Vision Loss and Age. [public domain]. https://archive.cdc.gov/#/details?url=https://www.cdc.gov/visionhealth/risk/age.htm ↵
- Fighting Blindness Canada. (2022, August 5). Tips to Protecting Children’s Vision for Back to School ↵
- California Department of Education . (2024). Special Education Enrollment by Age and Disability Statewide Report. https://data1.cde.ca.gov/dataquest/SpecEd/SpecEd1.asp?cChoice=SpecEd1&cYear=2018-19&cLevel=State&cTopic=SpecEd&myTimeFrame=S&submit1=Submit&ReptCycle=December ↵
- Head Start Early Childhood Learning & Knowledge Center. (2021). Infographic: Young Children with Special Needs. [public domain]. https://eclkc.ohs.acf.hhs.gov/children-disabilities/publication/infographic-young-children-disabilities ↵
- U.S. Department of Education. (n.d.). About IDEA. [public domain]. https://sites.ed.gov/idea/about-idea/ ↵
- Image by California Department of Education. (2012). California Infant/Toddler Curriculum Framework. https://www.cde.ca.gov/sp/cd/re/documents/itcurriculumframework.pdf ↵
- Head Start Early Childhood Learning & Knowledge Center. (2021). Infographic: Young Children with Special Needs. [public domain]. https://eclkc.ohs.acf.hhs.gov/children-disabilities/publication/infographic-young-children-disabilities ↵
- U.S. Department of Health and Human Services and the U.S. Department of Education. (2015). Policy Statement on Inclusion of Children with Disabilities in Early Childhood Programs. [public domain]. https://www2.ed.gov/policy/speced/guid/earlylearning/joint-statement-full-text.pdf ↵

