Chapter 8: The Circulatory System
Learning Objectives
By the end of this section, you will be able to:
- Describe the function of the circulatory system
- Describe the cardiac cycle
- Explain how blood flows through the body
- List the basic components of the blood
Animals are complex multicellular organisms that require a mechanism for transporting nutrients throughout their bodies and removing wastes. The human circulatory system has a complex network of blood vessels that reach all parts of the body. This extensive network supplies the cells, tissues, and organs with oxygen and nutrients, and removes carbon dioxide and waste compounds.
The medium for transport of gases and other molecules is the blood, which continually circulates through the system. Pressure differences within the system cause the movement of the blood and are created by the pumping of the heart.
Gas exchange between tissues and the blood is an essential function of the circulatory system. In humans and other mammals, blood absorbs oxygen and releases carbon dioxide in the lungs. Thus the circulatory and respiratory system, whose function is to obtain oxygen and discharge carbon dioxide, work in tandem.
The Circulatory System
The circulatory system is a network of vessels—the arteries, veins, and capillaries—and a pump, the heart. In all vertebrate organisms this is a closed-loop system, in which the blood is largely separated from the body’s other extracellular fluid compartment, the interstitial fluid, which is the fluid bathing the cells. Blood circulates inside blood vessels and circulates in one direction from the heart around one of two circulatory routes, then returns to the heart again.
The Heart
The heart is a complex muscle that consists of two pumps: one that pumps blood through pulmonary circulation to the lungs, and the other that pumps blood through systemic circulation to the rest of the body’s tissues (and the heart itself) (Figure 8.1).
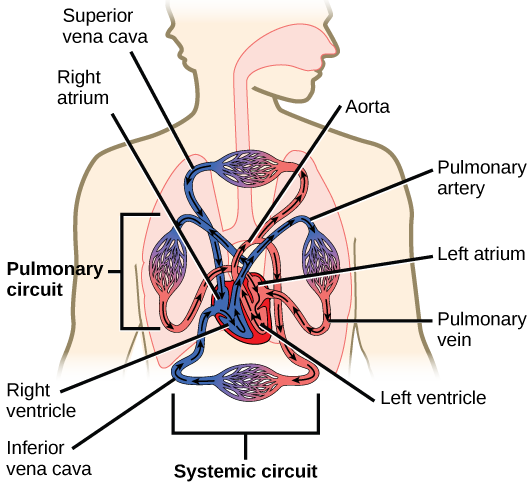
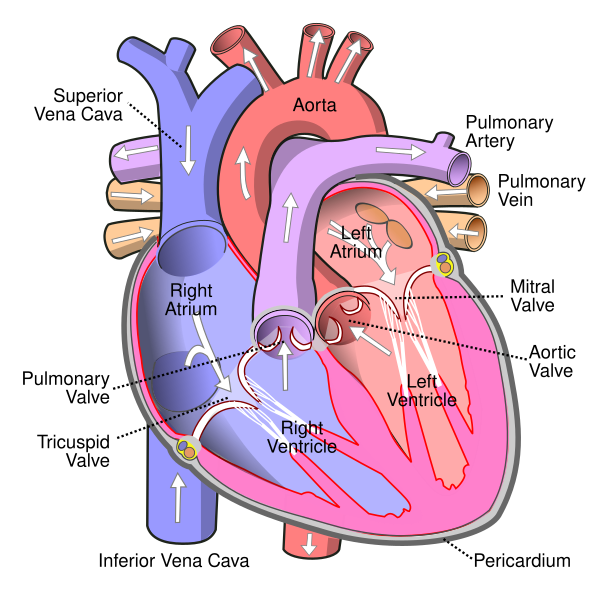
The heart is asymmetrical, with the left side being larger than the right side, correlating with the different sizes of the pulmonary and systemic circuits (Figure 8.1). In humans, the heart is about the size of a clenched fist; it is divided into four chambers: two atria and two ventricles. There is one atrium and one ventricle on the right side and one atrium and one ventricle on the left side. The right atrium receives deoxygenated (oxygen-poor) blood from the systemic circulation through the major veins: the superior vena cava, which drains blood from the head and from the veins that come from the arms, as well as the inferior vena cava, which drains blood from the veins that come from the lower organs and the legs. This deoxygenated blood then passes to the right ventricle through the tricuspid valve, which prevents the backflow of blood. After it is filled, the right ventricle contracts, pumping the blood to the lungs for reoxygenation. The left atrium receives the oxygen-rich blood from the lungs. This blood passes through the bicuspid valve to the left ventricle where the blood is pumped into the aorta. The aorta is the major artery of the body, taking oxygenated blood to the organs and muscles of the body. This pattern of pumping is referred to as double circulation and is found in all mammals. (Figure 8.2).
The Cardiac Cycle
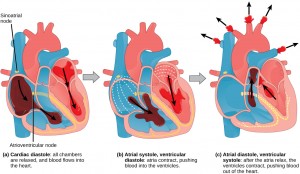
The main purpose of the heart is to pump blood through the body. It does so in a repeating sequence called the cardiac cycle. The cardiac cycle is the flow of blood through the heart coordinated by electrochemical signals that cause the heart muscle to contract and relax. In each cardiac cycle, a sequence of contractions pushes out the blood, pumping it through the body; this is followed by a relaxation phase, where the heart fills with blood. These two phases are called the systole (contraction) and diastole (relaxation), respectively (Figure 8.3). The signal for contraction begins at a location on the outside of the right atrium. The electrochemical signal moves from there across the atria causing them to contract. The contraction of the atria forces blood through the valves into the ventricles. Closing of these valves caused by the contraction of the ventricles produces a “lub” sound. The signal has, by this time, passed down the walls of the heart, through a point between the right atrium and right ventricle. The signal then causes the ventricles to contract. The ventricles contract together forcing blood into the aorta and the pulmonary arteries. Closing of the valves to these arteries caused by blood being drawn back toward the heart during ventricular relaxation produces a monosyllabic “dub” sound.
The pumping of the heart is a function of the cardiac muscle cells, or cardiomyocytes, that make up the heart muscle. Cardiomyocytes are distinctive muscle cells that are striated like skeletal muscle but pump rhythmically and involuntarily like smooth muscle; adjacent cells are connected by intercalated disks found only in cardiac muscle. These connections allow the electrical signal to travel directly to neighboring muscle cells.
The electrical impulses in the heart produce electrical currents that flow through the body and can be measured on the skin using electrodes. This information can be observed as an electrocardiogram (ECG) a recording of the electrical impulses of the cardiac muscle.
Blood Vessels
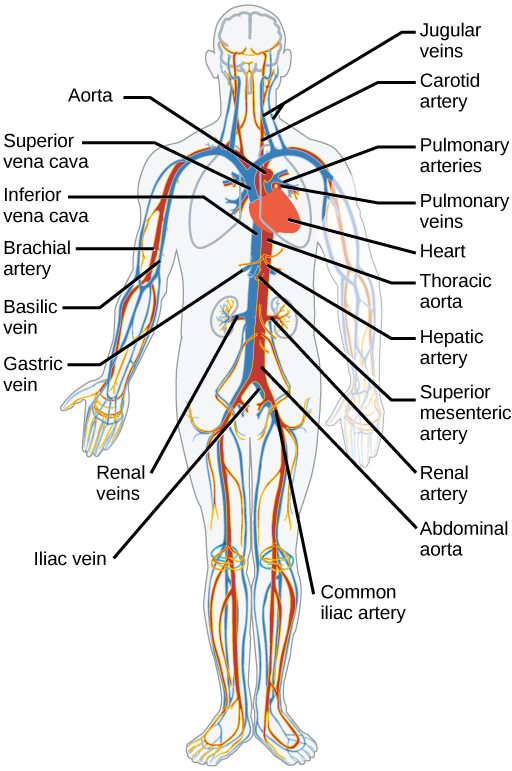
The blood from the heart is carried through the body by a complex network of blood vessels (Figure 8.4). Arteries take blood away from the heart. The main artery of the systemic circulation is the aorta; it branches into major arteries that take blood to different limbs and organs. The aorta and arteries near the heart have heavy but elastic walls that respond to and smooth out the pressure differences caused by the beating heart. Arteries farther away from the heart have more muscle tissue in their walls that can constrict to affect flow rates of blood. The major arteries diverge into minor arteries, and then smaller vessels called arterioles, to reach more deeply into the muscles and organs of the body.
Arterioles diverge into capillary beds. Capillary beds contain a large number, 10’s to 100’s of capillaries that branch among the cells of the body. Capillaries are narrow-diameter tubes that can fit single red blood cells and are the sites for the exchange of nutrients, waste, and oxygen with tissues at the cellular level. Fluid also leaks from the blood into the interstitial space from the capillaries. The capillaries converge again into venules that connect to minor veins that finally connect to major veins. Veins are blood vessels that bring blood high in carbon dioxide back to the heart. Veins are not as thick-walled as arteries, since pressure is lower, and they have valves along their length that prevent backflow of blood away from the heart. The major veins drain blood from the same organs and limbs that the major arteries supply.
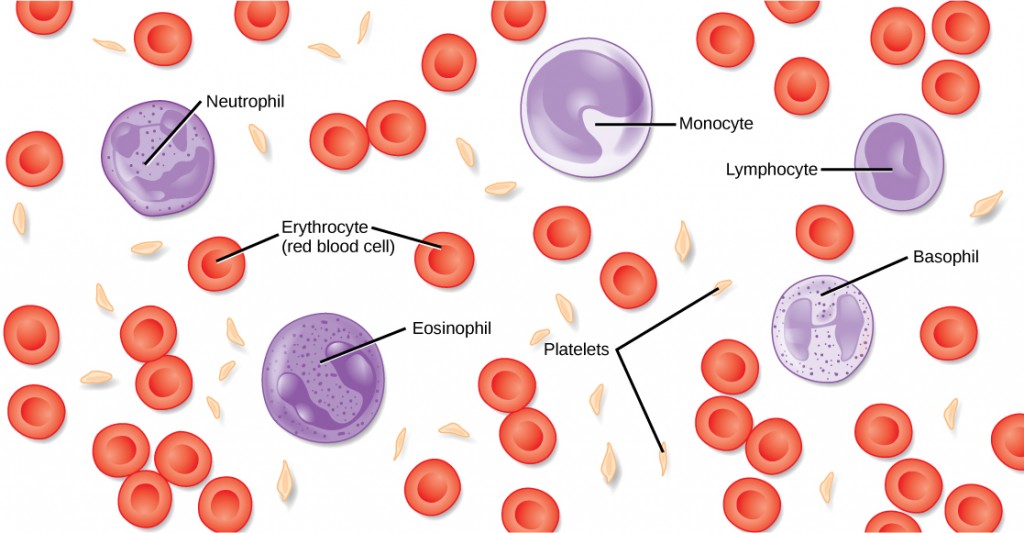
Blood
Hemoglobin is responsible for distributing oxygen, and to a lesser extent, carbon dioxide, throughout the circulatory system. The blood is more than the proteins, though. Blood is actually a term used to describe the liquid that moves through the vessels and includes plasma (the liquid portion, which contains water, proteins, salts, lipids, and glucose) and the cells (red and white cells) and cell fragments called platelets. Blood plasma is actually the dominant component of blood and contains the water, proteins, electrolytes, lipids, and glucose. The cells are responsible for carrying the gases (red cells) and immune response (white). The platelets are responsible for blood clotting. In humans, cellular components make up approximately 45 percent of the blood and the liquid plasma 55 percent. Blood is 20 percent of a person’s extracellular fluid and eight percent of weight.
The Role of Blood in the Body
Blood is important for regulation of the body’s systems and homeostasis (Figure 8.5). Blood helps maintain homeostasis by stabilizing pH, temperature, osmotic pressure, and by eliminating excess heat. Blood supports growth by distributing nutrients and hormones, and by removing waste. Blood plays a protective role by transporting clotting factors and platelets to prevent blood loss and transporting the disease-fighting agents or white blood cells to sites of infection.
Red Blood Cells
Red blood cells, or erythrocytes (erythro- = “red”; -cyte = “cell”), are specialized cells that circulate through the body delivering oxygen to cells. They are formed from stem cells in the bone marrow. In humans, red blood cells are small biconcave cells that at maturity do not contain a nucleus or mitochondria and are only 7–8 µm in size.
The red coloring of blood comes from the iron-containing protein hemoglobin. The principal job of this protein is to carry oxygen, but it also transports carbon dioxide as well. Hemoglobin is packed into red blood cells at a rate of about 250 million molecules of hemoglobin per cell. Each hemoglobin molecule binds four oxygen molecules so that each red blood cell carries one billion molecules of oxygen. There are approximately 25 trillion red blood cells in the five liters of blood in the human body, which could carry up to 25 sextillion (25 × 1021) molecules of oxygen in the body at any time.
White Blood Cells
White blood cells, also called leukocytes (leuko = white), make up approximately one percent by volume of the cells in blood. The role of white blood cells is very different than that of red blood cells: they are primarily involved in the immune response to identify and target pathogens, such as invading bacteria, viruses, and other foreign organisms. White blood cells are formed continually; some only live for hours or days, but some live for years.
Platelets and Coagulation Factors
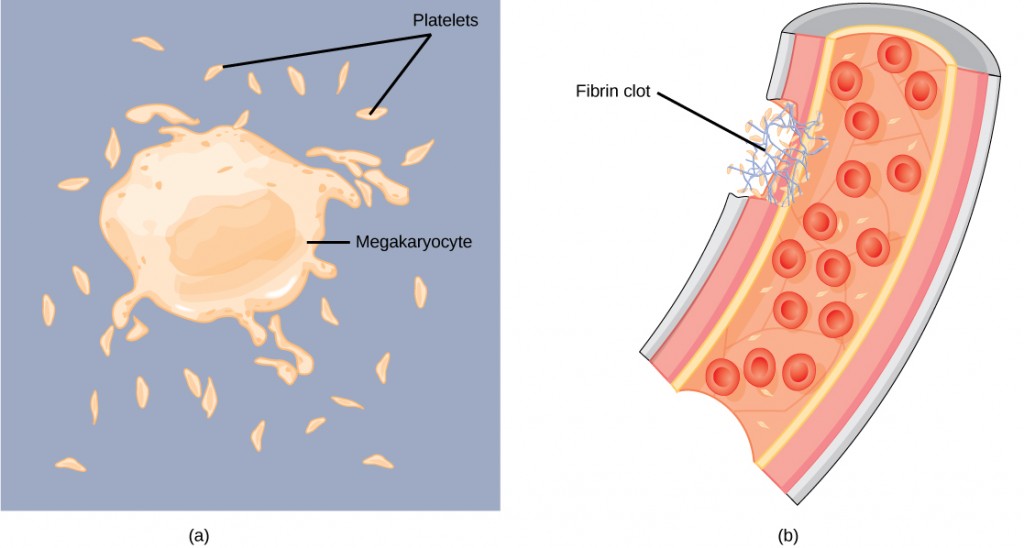
Blood must clot to heal wounds and prevent excess blood loss. Small cell fragments called platelets (thrombocytes) are attracted to the wound site where they adhere by extending many projections and releasing their contents. These contents activate other platelets and also interact with other coagulation factors, which convert fibrinogen, a water-soluble protein present in blood serum into fibrin (a non-water soluble protein), causing the blood to clot. Many of the clotting factors require vitamin K to work, and vitamin K deficiency can lead to problems with blood clotting. Many platelets converge and stick together at the wound site forming a platelet plug (also called a fibrin clot) (Figure 8.6b). The plug or clot lasts for a number of days and stops the loss of blood. Platelets are formed from the disintegration of larger cells called megakaryocytes (Figure 8.6a).
Plasma
The liquid component of blood is called plasma, and it is separated by spinning or centrifuging the blood at high rotations (3000 rpm or higher). The blood cells and platelets are separated by centrifugal forces to the bottom of a specimen tube. The upper liquid layer, the plasma, consists of 90 percent water along with various substances required for maintaining the body’s pH, osmotic load, and for protecting the body. The plasma also contains the coagulation factors and antibodies. The plasma component of blood without the coagulation factors is called the serum.
Blood Types Related to Proteins on the Surface of the Red Blood Cells
Red blood cells are coated in antigens whose composition is determined by genetics, which have evolved over time. In humans, the different surface antigens are grouped into 24 different blood groups with more than 100 different antigens on each red blood cell. The two most well known blood groups are the ABO (Figure 8.7) and Rh systems.
The surface antigens in the ABO blood group are glycolipids, called antigen A and antigen B. People with blood type A have antigen A, those with blood type B have antigen B, those with blood type AB have both antigens, and people with blood type O have neither antigen. Antibodies called agglutinogens are found in the blood plasma and react with the A or B antigens, if the two are mixed. When type A and type B blood are combined, agglutination (clumping) of the blood occurs because of antibodies in the plasma that bind with the opposing antigen This causes clots that coagulate in the kidney causing kidney failure. Type O blood has neither A or B antigens, and therefore, type O blood can be given to all blood types. Type O negative blood is the universal donor. Type AB positive blood is the universal acceptor because it has both A and B antigen. The ABO blood groups were discovered in 1900 and 1901 by Karl Landsteiner at the University of Vienna.
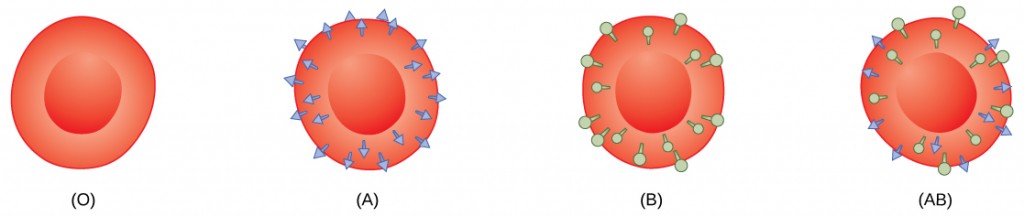
The Rh blood group was first discovered in Rhesus monkeys. Most people have the Rh antigen (Rh+) and do not have anti-Rh antibodies in their blood. The few people who do not have the Rh antigen and are Rh– can develop anti-Rh antibodies if exposed to Rh+ blood. This can happen after a blood transfusion or after an Rh– woman has an Rh+ baby. The first exposure does not usually cause a reaction; however, at the second exposure, enough antibodies have built up in the blood to produce a reaction that causes agglutination and breakdown of red blood cells. An injection can prevent this reaction.
Summary
The human circulatory system consists of a network of vessels containing blood that circulates because of pressure differences generated by the heart. The heart contains two pumps that move blood through the pulmonary and systemic circulations. There is one atrium and one ventricle on the right side and one atrium and one ventricle on the left side. The pumping of the heart is a function of muscle cells that are striated like skeletal muscle but pump rhythmically and involuntarily like smooth muscle. The electrochemical signal causes the two atria to contract in unison, then the signal causes the ventricles to contract. The blood from the heart is carried through the body by a complex network of blood vessels. Arteries take blood away from the heart, and veins bring blood back to the heart.
Specific components of the blood include red blood cells, white blood cells, platelets, and the plasma, which contains coagulation factors and serum. Blood is important for regulation of the body’s pH, temperature, osmotic pressure, the circulation of nutrients and removal of waste, the distribution of hormones from endocrine glands, and the elimination of excess heat. It also contains components for blood clotting. Red blood cells are specialized cells that contain hemoglobin and circulate through the body delivering oxygen to cells. White blood cells are involved in the immune response to identify and target invading bacteria, viruses, and other foreign organisms. They also recycle waste components, such as old red blood cells. Platelets and blood clotting factors cause the change of the soluble protein fibrinogen to the insoluble protein fibrin at a wound site forming a plug. Plasma consists of 90 percent water along with various substances, such as coagulation factors and antibodies.
Exercises
- Which of the following statements about the circulatory system is false?
- Blood in the pulmonary vein is deoxygenated.
- Blood in the inferior vena cava is deoxygenated.
- Blood in the pulmonary artery is deoxygenated.
- Blood in the aorta is oxygenated.
- Where does the right ventricle send blood?
- the head
- the upper body
- the lungs
- the lower body
- During the systolic phase of the cardiac cycle, the heart is ________.
- contracting
- relaxing
- contracting and relaxing
- filling with blood
- How do arteries differ from veins?
- Arteries have thicker wall layers to accommodate the changes in pressure from the heart.
- Arteries carry blood.
- Arteries have thinner wall layers and valves and move blood by the action of skeletal muscle.
- Arteries are thin walled and are used for gas exchange.
- Describe the cardiac cycle.
- White blood cells
- can be classified as granulocytes or agranulocytes
- defend the body against bacteria and viruses
- are also called leucocytes
- All of the above
- Platelet plug formation occurs at which point?
- when large megakaryocytes break up into thousands of smaller fragments
- when platelets are dispersed through the blood stream
- when platelets are attracted to a site of blood vessel damage
- none of the above
- In humans, the plasma comprises what percentage of the blood?
- 45 percent
- 55 percent
- 25 percent
- 90 percent
- The red blood cells of birds differ from mammalian red blood cells because:
- they are white and have nuclei
- they do not have nuclei
- they have nuclei
- they fight disease
- Describe the cause of different blood type groups.
- List some of the functions of blood in the body.
- How does the lymphatic system work with blood flow?
Answers
- A
- C
- A
- A
- The heart receives an electrical signal triggering the cardiac muscle cells in the atria to contract. The signal pauses before passing onto the ventricles so the blood is pumped through the body. This is the systolic phase. The heart then relaxes in diastole and fills again with blood.
- D
- C
- B
- C
- Red blood cells are coated with proteins called antigens made of glycolipids and glycoproteins. When type A and type B blood are mixed, the blood agglutinates because of antibodies in the plasma that bind with the opposing antigen. Type O blood has no antigens. The Rh blood group has either the Rh antigen (Rh+) or no Rh antigen (Rh–).
- Blood is important for regulation of the body’s pH, temperature, and osmotic pressure, the circulation of nutrients and removal of wastes, the distribution of hormones from endocrine glands, the elimination of excess heat; it also contains components for the clotting of blood to prevent blood loss. Blood also transports clotting factors and disease-fighting agents.
- Lymph capillaries take fluid from the blood to the lymph nodes. The lymph nodes filter the lymph by percolation through connective tissue filled with white blood cells. The white blood cells remove infectious agents, such as bacteria and viruses, to clean the lymph before it returns to the bloodstream.
Key Takeaways
aorta: the major artery that takes blood away from the heart to the systemic circulatory system
artery: a blood vessel that takes blood away from the heart
atrium: (plural: atria) a chamber of the heart that receives blood from the veins
bicuspid valve: a one-way opening between the atrium and the ventricle in the left side of the heart
capillary: the smallest blood vessel that allows the passage of individual blood cells and the site of diffusion of oxygen and nutrient exchange
cardiac cycle: the filling and emptying the heart of blood caused by electrical signals that cause the heart muscles to contract and relax
diastole: the relaxation phase of the cardiac cycle when the heart is relaxed and the ventricles are filling with blood
electrocardiogram (ECG): a recording of the electrical impulses of the cardiac muscle
hemoglobin: a protein found in red blood cells responsible for transporting oxygen and carbon dioxide
inferior vena cava: the major vein of the body returning blood from the lower parts of the body to the right atrium
plasma: liquid component of blood that is left after the cells are removed
platelet: small cellular fragment that collects at wounds, cross-reacts with clotting factors, and forms a plug to prevent blood loss
pulmonary circulation: the flow of blood away from the heart through the lungs where oxygenation occurs and then back to the heart
red blood cell: small biconcave cell without mitochondria that is packed with hemoglobin, giving the cell its red color; transports oxygen through the body
serum: plasma without the coagulation factors
superior vena cava: the major vein of the body returning blood from the upper part of the body to the right atrium
systemic circulation: the flow of blood away from the heart to the brain, liver, kidneys, stomach, and other organs, the limbs, and the muscles of the body, and then back to the heart
systole: the contraction phase of cardiac cycle when the ventricles are pumping blood into the arteries
tricuspid valve: a one-way opening between the atrium and the ventricle in the right side of the heart
vein: a blood vessel that brings blood back to the heart
ventricle: (of the heart) a large chamber of the heart that pumps blood into arteries
white blood cell: large cell with nuclei of which there are many types with different roles including the protection of the body from viruses and bacteria, and cleaning up dead cells and other waste
Media Attributions
Figure 8. 2 Wapcalet. (2020). Diagram of the human heart. Wikipedia. CC BY

